Emergency Medicine: All Areas
Emergency Medicine 12
489 - Delays to Pelvic Ultrasound in the Pediatric Emergency Department
Publication Number: 489.311
.jpg)
Louise Malburg, MD (she/her/hers)
Clinical Fellow
Washington University in St. Louis School of Medicine
St Louis, Missouri, United States
Presenting Author(s)
Background:
Adnexal torsion (AT) in the pediatric population is a rare diagnosis that may have a significant impact on ovarian function and future fertility if not promptly recognized and treated. AT is diagnosed by transvaginal (TVUS) or transabdominal (TAUS) pelvic ultrasound, although the latter is more commonly used in pediatrics. Due to the need for a full bladder prior to TAUS, the diagnosis and management of AT is often delayed.
Objective:
The primary objectives of this study were to 1) identify delays in pediatric patients undergoing TAUS in the emergency department (ED), and to 2) determine the impact on ED length of stay (LOS) and time to definitive treatment of patients with confirmed AT.
Design/Methods:
This was a retrospective observational study of all female patients who presented to a tertiary care pediatric ED and had a TAUS for the evaluation of AT from 6/2018 - 3/2022. Only TAUS scans were included as TVUS are not performed at this institution. Demographics, clinical data, and operative reports were recorded after chart review. ED arrival, first provider evaluation (FPE), US order and start times, ED disposition and departure times were obtained from the medical record. Bladder filling methods were categorized as: oral (PO), intravenous fluids (IVF), urinary catheterization (UC). The median and interquartile range (IQR) for the clinical times were examined and compared using bivariate analyses.
Results:
700 encounters were included in the study. Demographic and clinical data are shown in Table 1. The mean age was 14.5 years (± 3.6) and most were post pubertal. The longest delay in the ED was the median time from US order to US start of 1.53 (IQR 0.85-2.38) hours (Table 2). When categorized by bladder filling method (Table 3), time to US was longest with IVF 1.83 (IQR 1.22-2.7) and combined IV/PO fluids 2.19 (IQR 1.71-3.28) hours. In the IVF group, a longer time to US correlated with multiple IV attempts and IV therapy consultation. Bladder filling via UC (n=30) was the shortest at 1.13 (IQR 0.65-2.07) hours. A total of 8.3% (n=58) of TAUS results were concerning for AT. After evaluation by subspecialists, 5.3% (n=37) went to the OR and 2.6% (n=18) had surgically confirmed AT. The median time from ED arrival to first incision time was 10.7 (IQR 6.5 - 18.5) hours.
Conclusion(s):
In the evaluation of suspected pediatric AT, time to diagnostic imaging caused the most significant delay in care. Time was longer if the bladder-filling method was IV or PO fluids and shorter with UC. Efforts focused on expanding use of TVUS in adolescents or reducing bladder-filling time may decrease time to AT diagnosis.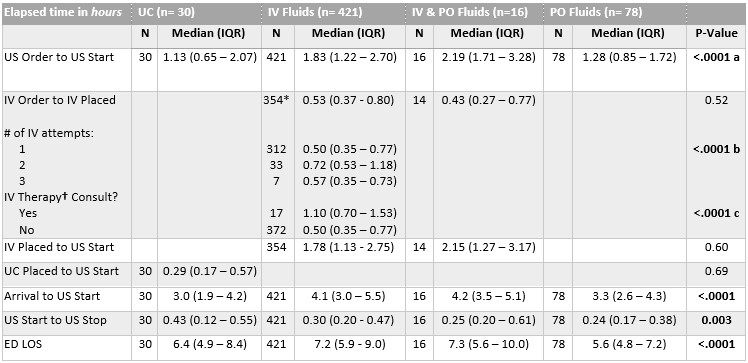
.jpg)
.jpg)
