Hypertension
Hypertension 2
19 - Association of HIV Disease Severity with Blood Pressure and Hypertension among Youth with Perinatally Acquired Infection
Publication Number: 19.322

Tammy M. Brady, MD, PhD (she/her/hers)
Associate Professor of Pediatrics
Johns Hopkins University
Baltimore, Maryland, United States
Presenting Author(s)
Background: HIV infection is a risk condition for accelerated atherosclerosis and is associated with a greater risk for cardiovascular (CV) events in adults. How perinatal HIV infection (PHIV) impacts blood pressure (BP) in youth is unclear.
Objective:
To determine if HIV disease severity is associated with BP among youth living with PHIV (YLPHIV).
Design/Methods:
A longitudinal analysis was conducted among YLPHIV enrolled in the Adolescent Master Protocol of the Pediatric HIV/AIDS Cohort Study, a prospective cohort study conducted at 15 US sites investigating the impact of PHIV on youth. Participants with ≥1 visit with BP measurements were included. At each visit, the mean of two automated BP measurements was calculated. Two BP outcomes were defined: 1) BP index (mean BP/age-sex-height specific 95th%ile BP; BP index ≥1 indicates a BP ≥95th %ile); 2) hypertensive BP (HTN) per 2017 Clinical Practice Guidelines. HIV severity up until the time of each BP measurement was determined by: 1) nadir CD4 count (< 200 vs ≥200 cells/mm3); 2) lifetime viral load (VL) burden, defined as percentage of time (%time) with suppressed VL (< 400 copies/mL) and time-averaged area under the VL curve [AUCt (AUC/individual time span)]; both included multiple imputation of missing VL values.
The association of HIV severity with outcomes was determined with repeated measures linear regression models using generalized estimating equations with robust variance for BP index and modified Poisson regression models for HTN, both unadjusted and adjusted for confounders.
Results:
Among 447 enrolled youth, mean nadir CD4 count was 365 cells/mm3, 27% had nadir CD4 < 200 cells/mm3, mean %time VL< 400 copies/mL was 39%, and mean AUCt was 3.4 Log₁₀ copies/mL. 90% were on combined antiretroviral therapy (ART), 69% were on a protease inhibitor, and 7% were on no ARV at a random timepoint. Sociodemographic characteristics, HIV disease severity and BP measures at a randomly selected datapoint are summarized in Table 1. There were no clinically meaningful associations of any HIV disease severity measure with BP indices (Table 2) or HTN (data not shown).
Conclusion(s):
In this cohort of youth with perinatal HIV infection, HIV disease severity was not associated with BP or HTN. Future studies are warranted to understand whether other HIV-related factors are associated with BP or HTN in YPHIV, or if traditional CVD risk factors confer greater CVD risk than HIV infection alone.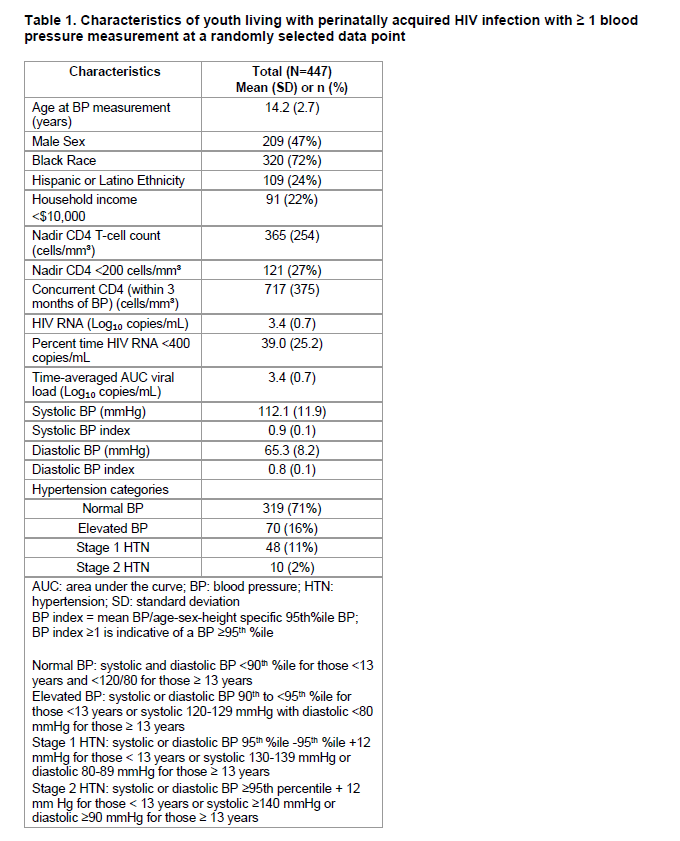
.png)
