Children with Chronic Conditions
Children with Chronic Conditions 3
79 - Comparison of Two Different Models of Inpatient Care for Medically Complex Children After Spinal Fusion Surgery
Publication Number: 79.305

Zachary Semenetz, MD (he/him/his)
Pediatrician
Nemours Children's Health - Primary Care, Newark
Wilmington, Delaware, United States
Presenting Author(s)
Background: For children with cerebral palsy and neuromuscular scoliosis, spinal fusion surgery is a common and effective treatment to correct the spinal deformity. This surgery is associated with significant risks including pulmonary compromise, infection, and gastrointestinal complications, often leading to prolonged hospitalization. Various models of postoperative care have been proposed to reduce the risk of complications and the length of stay.
Objective: The goal of this study was to assess differences between two different models of inpatient management for medically complex patients with neuromuscular scoliosis after spinal fusion surgery.
Design/Methods: We conducted a retrospective chart review of patients during a period of 5 years and 5 months to compare clinical outcomes between a hospitalist/orthopedics co-management team and a complex care team at a single institution. To account for baseline differences between treatment groups, we calculated propensity scores and used these as probability weights in generalized linear models.
Results:
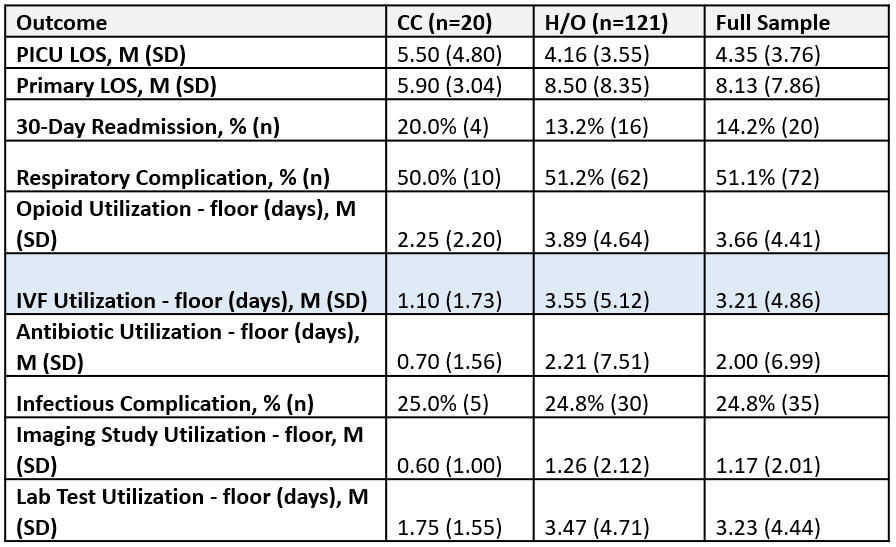
In bivariate analysis, prior to matching, there was a significantly lower intravenous fluid utilization for the complex care treatment group (n = 20) compared to the hospitalist/orthopedic service (n = 121) (1.1 vs 3.6 days; p = 0.040) while there was no statistically significant difference in length of stay (5.9 vs 8.5 days; p = 0.171), our primary outcome. After propensity score matching in generalized-linear models, the complex care treatment group had a shorter primary length of stay before (-2.60; p = 0.040) and after accounting for patient tracheostomy and G-tube dependence (-3.01; p = 0.034). After propensity score matching, the complex care treatment group also had significantly lower intravenous fluid utilization (-1.08; p = 0.002), antibiotic utilization (-1.77; p = 0.004), and lab test utilization (-0.76; p = 0.005) compared to the hospitalist/orthopedics treatment group. No significant difference between groups was seen for 30-day readmission rate (p = 0.619), respiratory complications (p = 0.741), opioid utilization (p = 0.088), infectious complications (p = 0.26), or imaging study utilization (p = 0.081).
Conclusion(s): In managing patients after spinal fusion surgery, the hospitalist/orthopedics co-management and complex care teams have comparable outcomes to prior studies. Management on the complex care team may have significant benefits for the most medically complex patients. 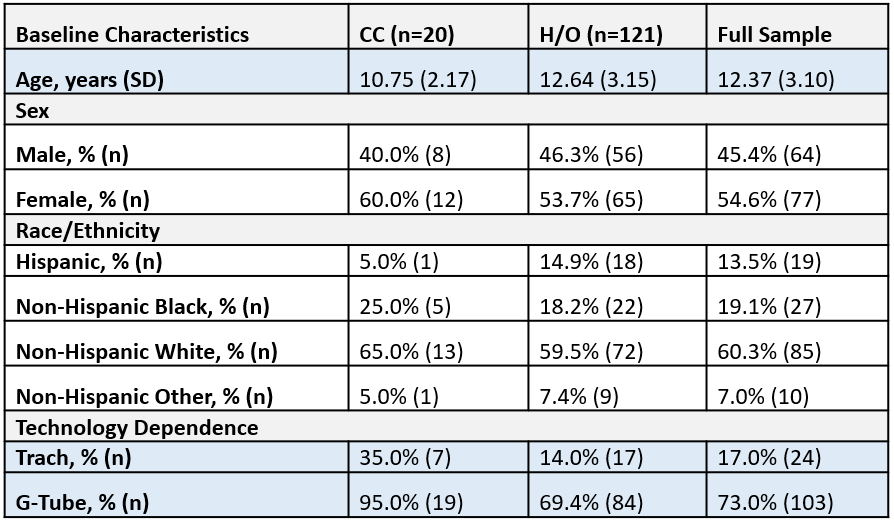
.png)
