Hypertension
Hypertension 1
10 - Discrepancy in recorded triage vs. clinic measured blood pressures among pediatric patients with obesity-related hypertension
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 10
Publication Number: 10.321
Publication Number: 10.321
William Wen, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Kevin Psoter, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Barry S. Solomon, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Elaine M. Urbina, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Tammy M. Brady, Johns Hopkins University, Baltimore, MD, United States
William Wen (he/him/his)
Medical Student
Johns Hopkins University School of Medicine
Baltimore, Maryland, United States
Presenting Author(s)
Background: Accurate triage blood pressure (BP) measurements are essential for clinical decision making and efficient clinic workflow. This can be challenging in busy settings, due to myriad factors.
Objective: Determine the agreement and diagnostic accuracy of triage BP measurements with standardized clinician measurements obtained in an obesity hypertension clinic (ReNEW Clinic).
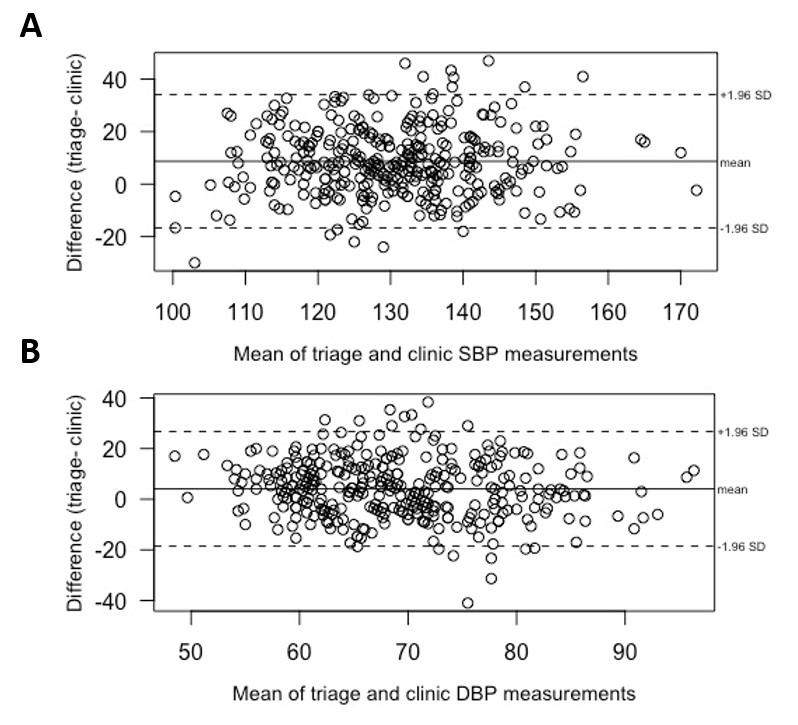
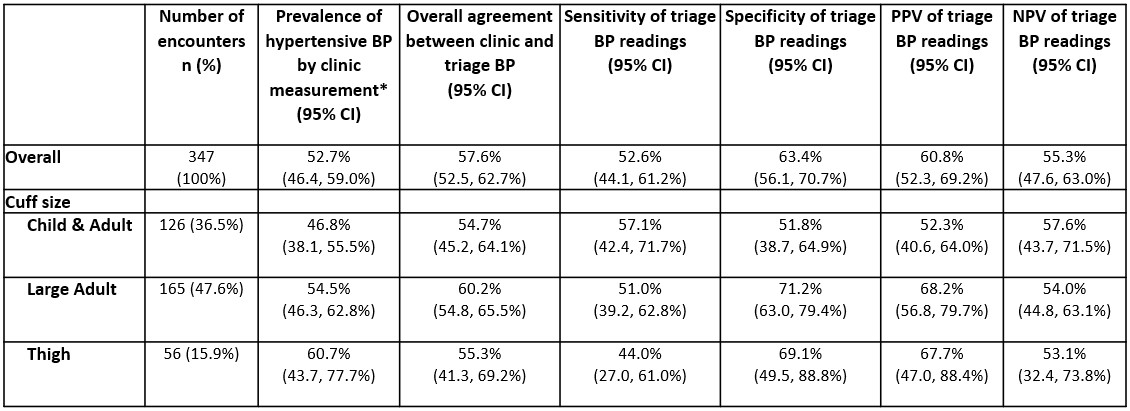
Design/Methods: This was a retrospective study of paired triage and clinician BP measurements obtained from patients 4-21 years old seen at the Johns Hopkins ReNEW clinic from 2015-2022. Triage BPs are measured by a medical assistant or nurse, often by automated device. Triplicate manual BP measurements are later obtained standardly by the clinic physician according to the 2017 AAP Clinical Practice Guidelines. Bland-Altman analyses accounting for multiple patient encounters determined mean differences and limits of agreement (LOA) between paired triage and mean of triplicate clinician BP measurements. GEE-based multivariable Poisson regression evaluated the relative risk (RR) of triage BP overestimation by ≥5 mmHg. Using clinician measurements as the reference standard, overall agreement, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of triage BP measurements were estimated.
Results: 130 unique participants with 347 clinic encounters were included in this analysis. Mean age at initial visit was 13.3 years (standard deviation = 3.94), 76% were Black race and 58% were male. Overall mean systolic BP (SBP) and diastolic BP (DBP) difference between triage and clinician measurements was 8.7 mmHg (95% LOA: -16.66, 34.07 mmHg) and 4.1 mmHg (95% LOA: -18.56, 26.68 mmHg), respectively (Figure). SBP was overestimated by ≥5 mmHg in 60.4% of triage measurements, while 46.8% of triage diastolic DBP were overestimated. Compared with BP measurements taken when a child/adult cuff was required, large adult [RR=1.49; 95% confidence interval (CI): 1.00, 2.21] and thigh cuffs (RR=1.94; 95% CI: 1.08, 3.51) were more likely to overestimate SBP, while thigh cuffs were more likely to overestimate DBP (RR=2.01; 95% CI: 1.02, 3.97 ). Overall agreement between triage and mean clinic measurements in identifying hypertensive BP was 57.6%. Sensitivity (52.6%), specificity (63.4%), PPV (60.8%), and NPV (55.3%) of triage measurements were low across all cuff sizes (Table).
Conclusion(s): Overall, we found a large discrepancy between triage and clinician BP measurements, especially among larger cuff sizes. These results reinforce the need for repeat BP measurements when triage BP is abnormal.