Hypertension
Hypertension 2
24 - Change in Cardiovascular Health in Youth with Hypertension Disorders Since 2015
Publication Number: 24.322

Carol Vincent, MD (she/her/hers)
pediatric nephrology fellow
Wake Forest Baptist Health - Brenner Children's Hospital
Winston Salem, North Carolina, United States
Presenting Author(s)
Background:
Obesity and associated metabolic complications dyslipidemia and hyperglycemia are cardiovascular health factors (CVHF) that are frequently seen as comorbidities to hypertension (HTN) in tertiary care clinics caring for youth with HTN disorders. The 2017 AAP HTN Clinical Practice Guideline (CPG) recommended that youth with HTN all receive dyslipidemia screening and those with obesity receive hyperglycemia screening, but it is unknown if this impacted the prevalence of CVHF in this population. With the COVID-19 pandemic that began in March 2020, obesity prevalence increased in the U.S. population overall though changes in CVHF prevalence in youth with HTN is not known.
Objective: To determine the relative risk of CVHF in youth with HTN disorders across eras: before 10/2017 and the 2017 AAP CPG (pre-CPG), between 10/2017 and 2/2020 (post-CPG), and on or after 3/2020 (pandemic).
Design/Methods:
This is an interim analysis using baseline data from the SUPERHERO Registry, a multisite retrospective cohort of youth referred for HTN disorders. Inclusion criteria were age < 19 years and HTN disorder identified by ICD-10 codes from 1/1/2015–12/31/2021 at an initial visit to a subspecialty clinic. Exclusion criteria were kidney failure on dialysis, kidney transplantation, or pregnancy by ICD-10 codes. Our exposure was era of initial visit. Our outcomes were CVHF: obesity (by BMI %ile), dyslipidemia (by ICD-10 codes), and hyperglycemia (by ICD-10 codes). We determined relative risk of CVHF progressing across eras (pre-CPG to post-CPG to pandemic) using unadjusted generalized linear models.
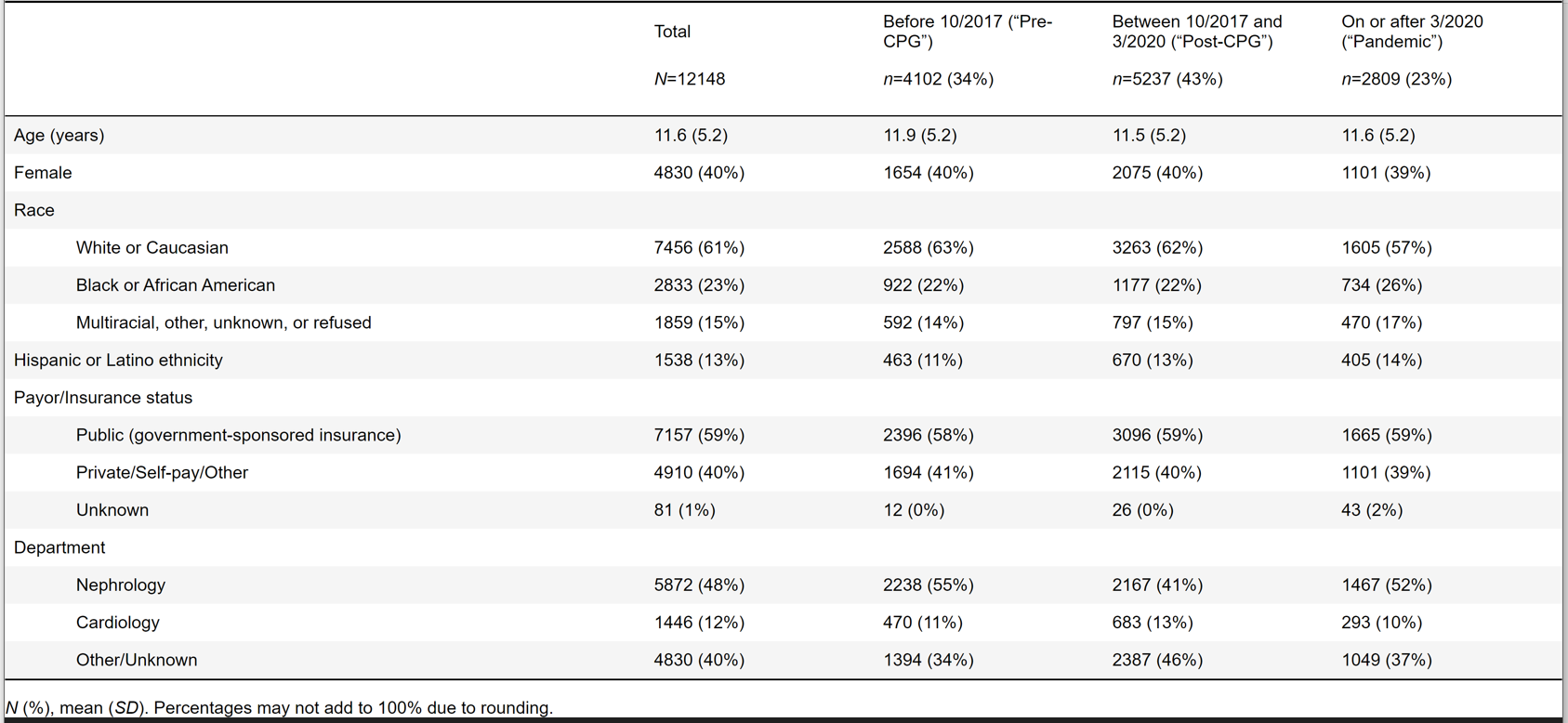
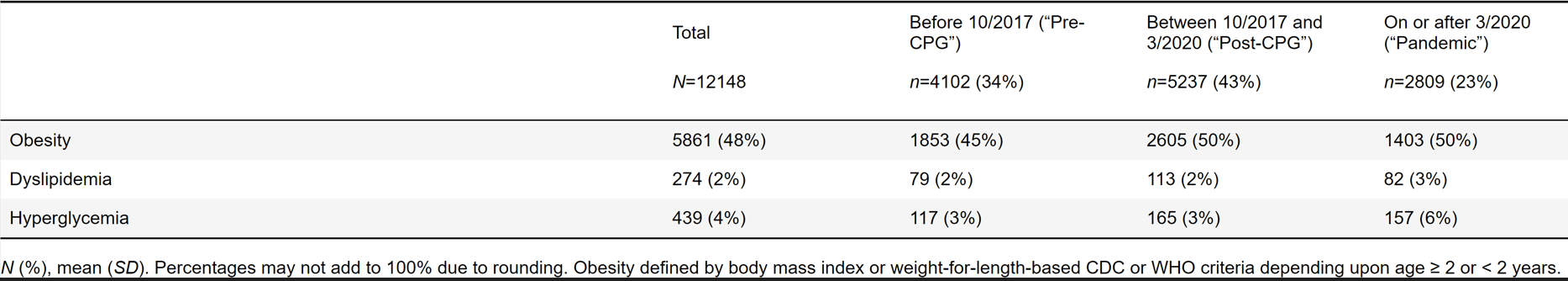
Results: Of 12148 participants, 34% had initial visit in pre-CPG, 43% in post-CPG, and 23% in pandemic eras (Table 1). Prevalence of CVHF by era is shown in Table 2. The risk of CVHF increased across eras with obesity, dyslipidemia, and hyperglycemia having relative risks of 1.07 (1.05, 1.10), 1.35 (1.15, 1.58), and 1.48 (1.31, 1.68), respectively.
Conclusion(s): Youth with HTN disorders were at increasing risk of worse CV health at initial visit with a subspecialist across eras, from pre-CPG to post-CPG to pandemic eras. While more widespread screening associated with the CPG may have contributed to better identification of dyslipidemia and hyperglycemia in youth with HTN, our findings also suggest that youth with HTN disorders in most recent era may be getting referred later possibly due to pandemic-related healthcare delays. Future steps include more complete CV health evaluation using laboratory values and following CVHF in youth with HTN disorders over time into a post-pandemic era.