Allergy, Immunology and Rheumatology
Allergy, Immunology, and Rheumatology
384 - The Impact of Geography on Food Insecurity in Pediatric Food Allergy Patients
Publication Number: 384.301
Maya M. Eldin (she/her/hers)
Medical Student
Dell Medical School at UT Austin
Austin, Texas, United States
Presenting Author(s)
Background:
Food insecurity affects approximately 7.6% of children in the United States and has increased due to the COVID-19 pandemic and rising food costs. Previous studies have shown higher rates of food insecurity in food allergic children, though data is limited. Additionally, geographic food access has been identified as a critical concept when designing policies to decrease food insecurity within a community and has historically been influenced by racial/ethnic disparities.
Objective:
The goal of this study was to investigate the relationship between geographic food access and food insecurity in an urban pediatric food allergy population as well as the roles of race/ethnicity and food allergy (FA) status.
Design/Methods:
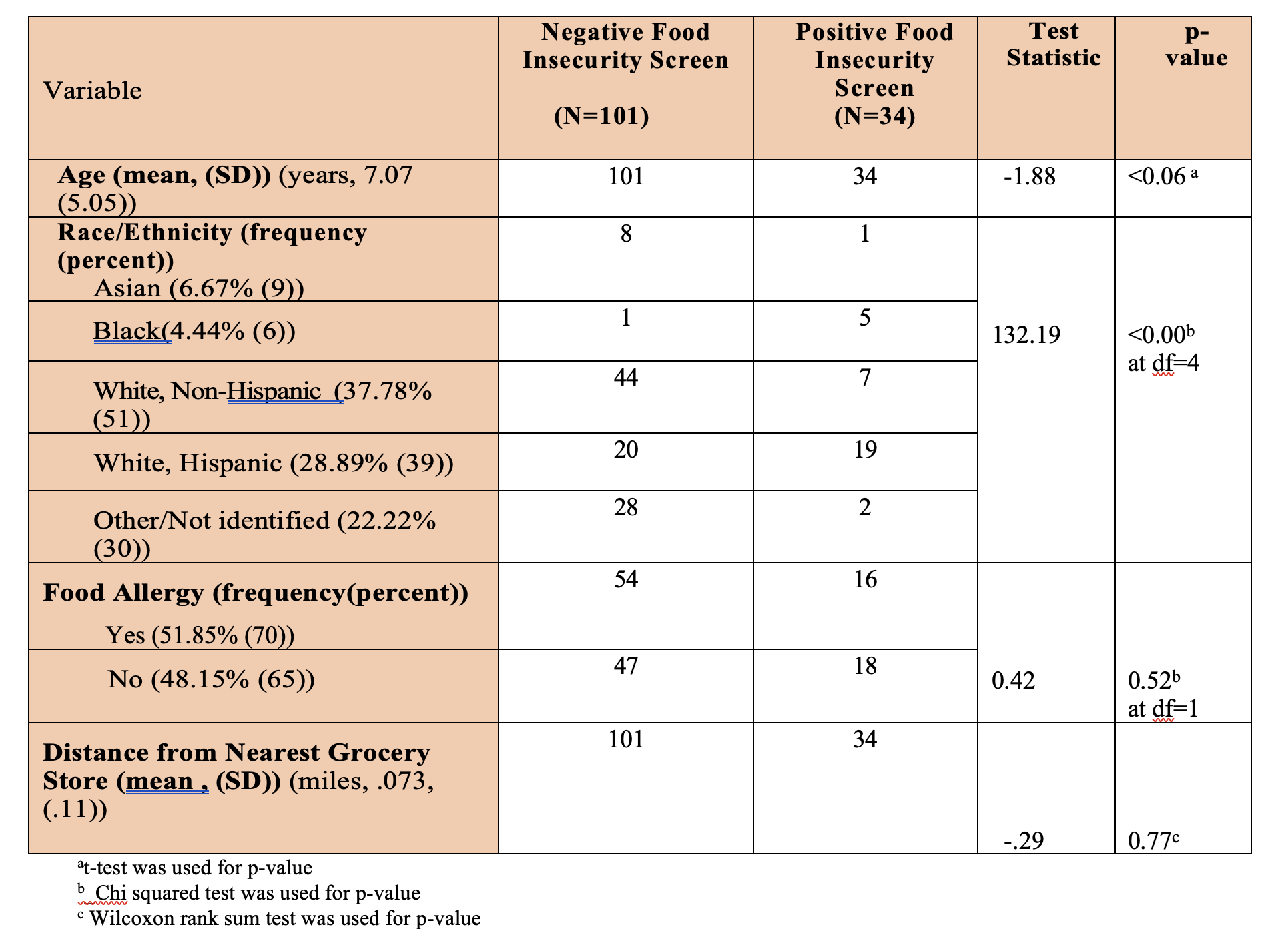
The validated two question Hunger Vital Sign™ questionnaire was offered in English and Spanish to parents of pediatric patients seen in a pediatric Allergy/Immunology clinic. Food insecurity is defined as a positive response to one of the two survey questions. Those with physician-diagnosed FA were asked a third question regarding access to allergen-free foods. Families that screened positive for food insecurity were provided with a list of local resources. Using participant zip codes, the distance between each participant's area of residence and the closest food retailer was calculated. Various statistical methods were used to analyze the impact of age, race/ethnicity, FA, and distance from nearest grocery store, on food insecurity status.
Results:
The response rate was 91%. 23% of families with physician-diagnosed food allergy were identified as food insecure. Black race was significantly associated with food insecurity. There were no association with age, FA status, or distance from nearest grocery store. Black subjects lived a greater distance from the nearest grocery store when compared with other race/ethnicity groups.
Conclusion(s):
23% of children with physician-diagnosed food allergy screened positive for food insecurity, which is higher than rates reported in the general pediatric population. Black race was significantly associated with food insecurity and increased distance from the nearest grocery store, although poor geographic food access was not independently associated with food insecurity. Future directions include the design of targeted interventions to aid families identified as food insecure as well as the development of an on-site food pantry with allergen-free foods. Subsequent analysis will further characterize the quality of food retail and accessibility in neighborhoods.