Neonatal Cardiac Physiology/Pathophysiology/Pulmonary Hypertension
Neonatal Cardiac Physiology/Pathophysiology/ Pulmonary Hypertension 2
230 - Hemodynamic Profile of Very Low Birth Weight Neonates with Sepsis-Related Hypotension
Publication Number: 230.33

Ashraf Kharrat, MD FRCPC MScHQ (she/her/hers)
Staff Neonatologist
Mount Sinai Hospital
Toronto, Ontario, Canada
Presenting Author(s)
Background:
Very low birth weight neonates (VLBW, BW < 1500 grams) frequently require vasopressors/inotropes for circulatory support during sepsis and have a high associated mortality rate; however, more data are needed for detailed delineation of their hemodynamic profile and association with mortality.
Objective:
To investigate comprehensive targeted neonatal echocardiography (TNE) findings in VLBWs needing vasopressors/inotropes for sepsis-related hypotension, and their association with mortality.
Design/Methods:
This retrospective study, conducted over 6-years, included all VLBWs who received vasopressors/inotropes and had a TNE performed within 72 hours of culture-positive sepsis onset at a tertiary NICU. Infants with genetic or cardiac anomalies (except PDA and PFO), and among whom TNE was unavailable, were excluded. Included TNEs were analyzed for conventional, tissue Doppler imaging (TDI) and speckle tracking echocardiography (STE) variables, representing left (LV) and right (RV) ventricular systolic and diastolic function and pulmonary hemodynamics. Infants surviving until discharge were compared to those who died. Receiver operating characteristic analysis was used to identify TNE variables with the largest area under the curve (AUC). Logistic regression (LR) was conducted to account for clinically relevant variables.
Results:
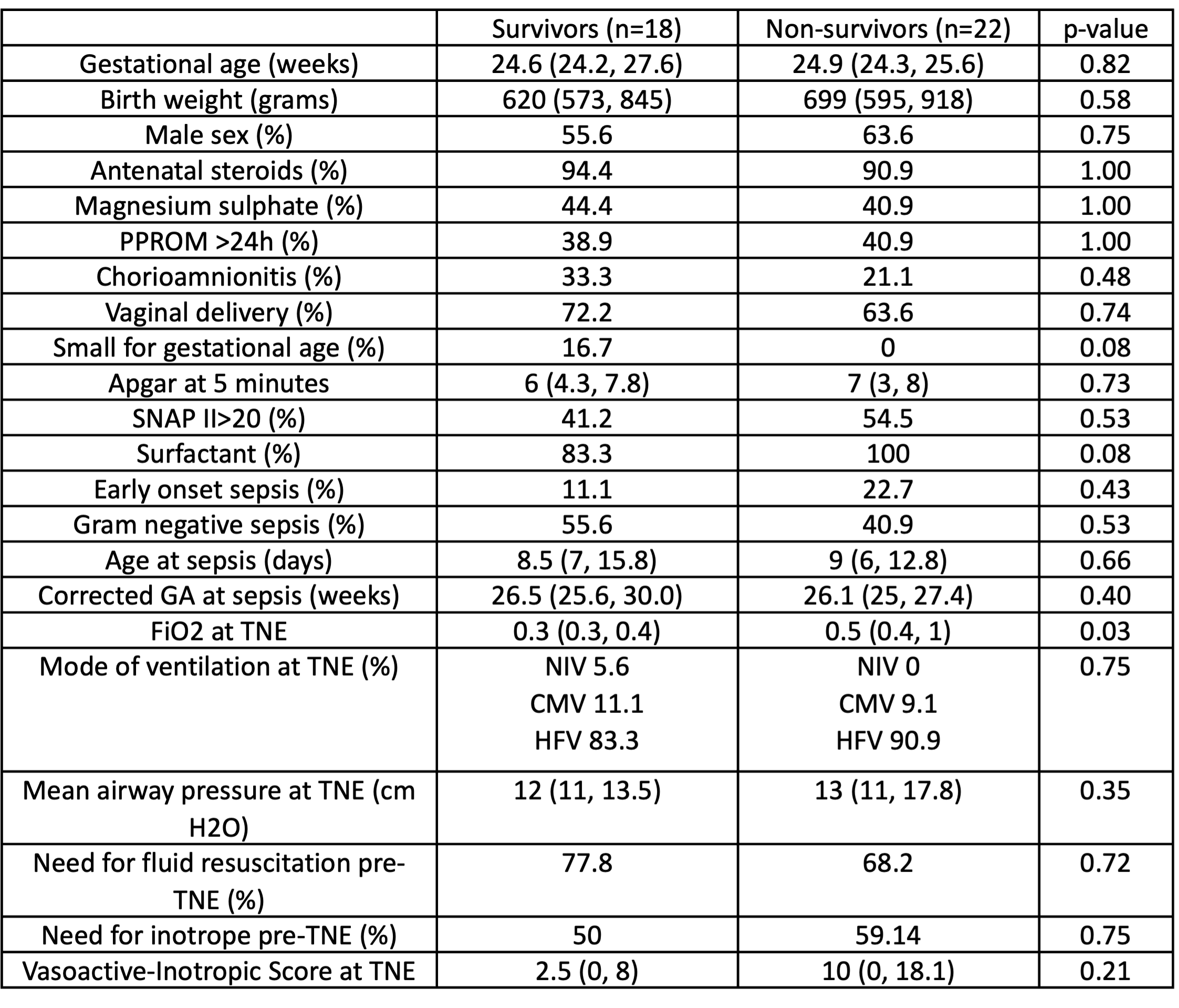
Of the 59 infants who received inotropes during sepsis, 40 had a TNE and were included; median GA, BW and age at sepsis were 24.7 (24.3, 26.0) weeks, 645 (578, 855) grams and 9 (6, 13) days, respectively. Infants who died before discharge (n=22, 55%) were similar in demographics and illness severity at TNE to those who survived (n=18), except for higher oxygen requirement (Table 1). Survivors had superior LV diastolic function on TDI and both LV systolic and diastolic function on STE (Table 2). Except higher mitral early inflow velocity and LV output, all conventional parameters as well as indices of RV function and pulmonary hemodynamics were similar. LV peak longitudinal strain (pLS) performed best for identifying mortality (AUC [95% CI] 0.81 [0.65, 0.96]) (Figure 1); pLS >-18.3 had a sensitivity and specificity of 90% and 71%, respectively. LV pLS remained associated with mortality on LR after accounting for GA, age at sepsis and gram-negative infection (adjusted odds ratio 1.28 [1.04 - 1.60]).
Conclusion(s):
Among VLBW infants needing vasopressors/inotropes during sepsis, use of TDI and STE can better delineate clinically significant alterations in cardiac function and may allow more informed risk stratification.
.png)
.png)
