Emergency Medicine: All Areas
Emergency Medicine 12
493 - Incidence and Management of Post-Tonsillectomy Hemorrhage in Pediatric Emergency Departments
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 493
Publication Number: 493.311
Publication Number: 493.311
David Vanderhoff, Boston Children's Hospital, Boston, MA, United States; Michael Monuteaux, Boston Children's Hospital, Boston, MA, United States; Joel Hudgins, Boston Children's Hospital, Milton, MA, United States; Susan Lipsett, Boston Children's Hospital, Boston, MA, United States

David I. Vanderhoff, MD (he/him/his)
Physician
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: More than 20,000 children undergo tonsillectomy in the United States annually, making it one of the most frequent pediatric surgical procedures performed. Post-tonsillectomy hemorrhage (PTH) is both a frequent and potentially catastrophic sequela, but there is limited evidence surrounding best practices for its management in the emergency department (ED).
Objective: To determine rates of pediatric ED visits for PTH and characterize variation in care.
Design/Methods: We conducted a retrospective cross-sectional analysis using the Pediatric Health Information Systems (PHIS) database to identify patients from 1 to 18 years old who underwent tonsillectomy between January 1, 2016 and September 30, 2021 (index visits). We then identified the subgroup of patients with an ED visit for PTH within 30 days of their index surgery (PTH visits). We examined demographic characteristics of index and PTH visits as well as the duration between index discharge and subsequent PTH visits. We also assessed variation in ED management across hospitals in diagnostic testing and management of the PTH group.
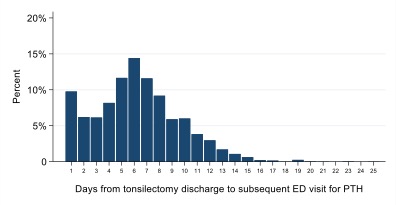
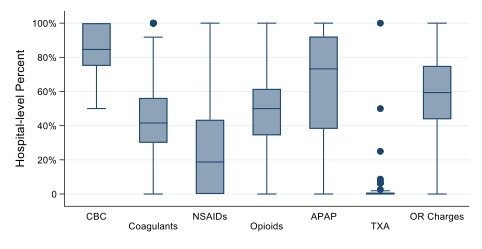
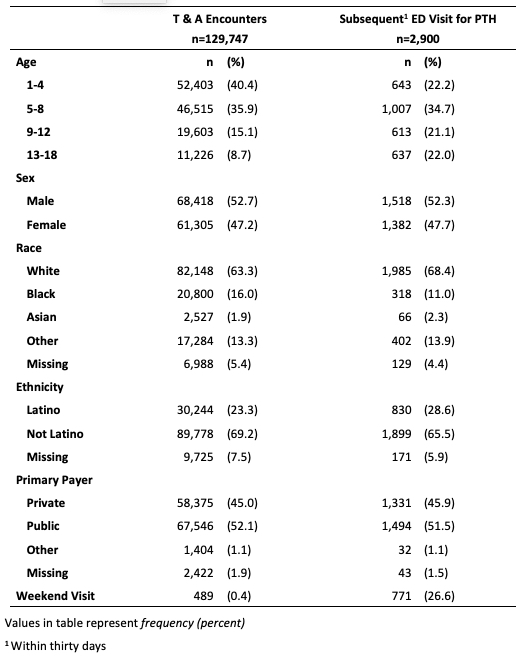
Results: We identified 129,747 patients with tonsillectomy from 2016 to 2021, of whom 2,900 (2.2%) presented for evaluation of PTH within 30 days of their index surgery. The number of PTH visits was highest among the 5-8 year old group. 13-18 year old patients comprised only 8.7% of index surgeries but 22% of PTH visits (Table 1). PTH ED visits were most common on day 6 after the index surgery, with 47.8% of visits clustered on days 5-8 (Figure 1). There was substantial variation among hospitals in diagnostic testing and management (Figure 2). Complete blood count (CBC) was the most common diagnostic test obtained, with median intra-hospital utilization in 85% of cases. Wide variation was seen in use of analgesics. Both opioid and non-steroidal anti-inflammatory drug (NSAID) usage, for example, varied from 0 to 100% by hospital, with median intra-hospital opioid usage in 50% of cases and median NSAID use of 19%. Use of novel therapeutics such as tranexamic acid is still low, with use reported in 2% of cases overall.
Conclusion(s): PTH remains a common side effect of tonsillectomy across all age groups. In addition, wide variation exists in the use of both diagnostic testing and therapeutics across pediatric hospitals. Development of guidelines for acute management of PTH will be vital to reduce variation in care for this common ED diagnosis.