Emergency Medicine: All Areas
Emergency Medicine 12
492 - Imaging Trends and Surgical Outcomes for Nephrolithiasis in the Pediatric Emergency Department
Publication Number: 492.311

Vidya R. Raghavan, MD (she/her/hers)
Fellow
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background:
The incidence of nephrolithiasis has increased dramatically over the past few decades in both adults and children. Renal-bladder ultrasound (US) is the preferred imaging modality in the pediatric population due to the avoidance of ionizing radiation despite non-contrast computed tomography (CT) having higher sensitivity and specificity for diagnosis.
Objective:
To evaluate current trends in imaging and rates of surgical intervention for pediatric nephrolithiasis presenting to the emergency department (ED).
Design/Methods:
We performed a multicenter, retrospective, cross-sectional analysis using the Pediatric Health Information System (PHIS) database. We included ED encounters for children age 1 to 21 with a diagnosis of nephrolithiasis using ICD-9 and 10 codes from 2010 to 2021. Children who had no imaging study performed, renal complex chronic conditions, transfers, and in-hospital mortality, as well as hospitals with incomplete data, were excluded. Variability in rates of CT imaging across hospitals was analyzed using the Wald test. Hospital-level analysis was performed by first grouping hospitals in quartiles based on rates of CT use. We then estimated a logistic model with surgery at the index visit as the dependent variable and hospital-level CT quartile as independent variable, adjusting for demographic and clinical management factors (administration of opioids, intravenous fluids and antibiotics). Another logistic model was estimated to assess the risk of surgery in the 6 months after the index visit.
Results:
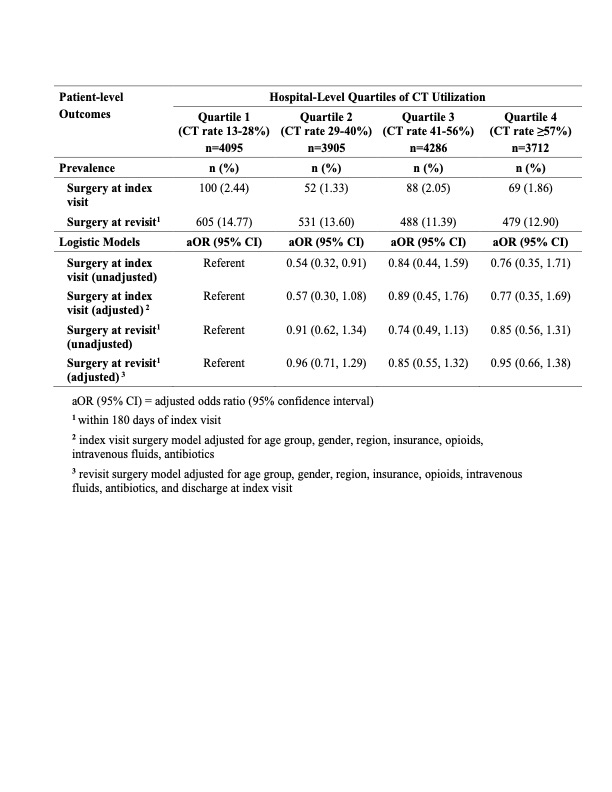
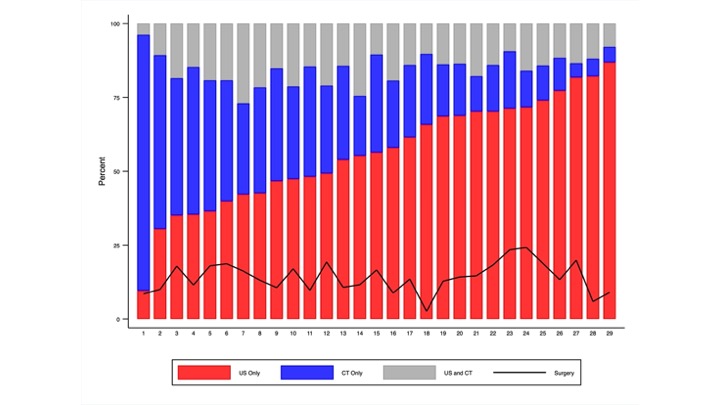
We identified 15,998 ED visits (median age 15 years, 59% female) across 29 different hospitals (Table 1). There was statistically significant variation in rates of CT across all hospitals (range 13-90%; p< 0.001, Figure 1). Surgery rates at the index visit were 1.33-2.44% while revisit surgery rates were 11.39-14.77% within the hospital quartiles. After adjusting for demographic and clinical factors, there were no differences in the odds of surgery based on hospital-level CT rate. Similarly, no significant differences were detected in the odds of revisit surgery (Table 2).
Conclusion(s):
In this hospital-level analysis of imaging for pediatric nephrolithiasis, CT utilization in the ED was not associated with increased rates of surgery at either the index hospitalization or within the 6-month period following the ED encounter. These findings suggest that opportunities exist to reduce CT utilization for children with nephrolithiasis..jpg)