Quality Improvement/Patient Safety: All Areas
QI 5: Quality Measures, Family Centered & Inpatient QI
245 - Enhancing Equity in Patient and Family Inpatient Safety Reporting
Publication Number: 245.451
- NB
Naomi S. Bardach, MD MAS (she/her/hers)
Professor of Pediatrics and Health Policy
UCSF Benioff Children's Hospital San Francisco
SF, California, United States
Presenting Author(s)
Background:
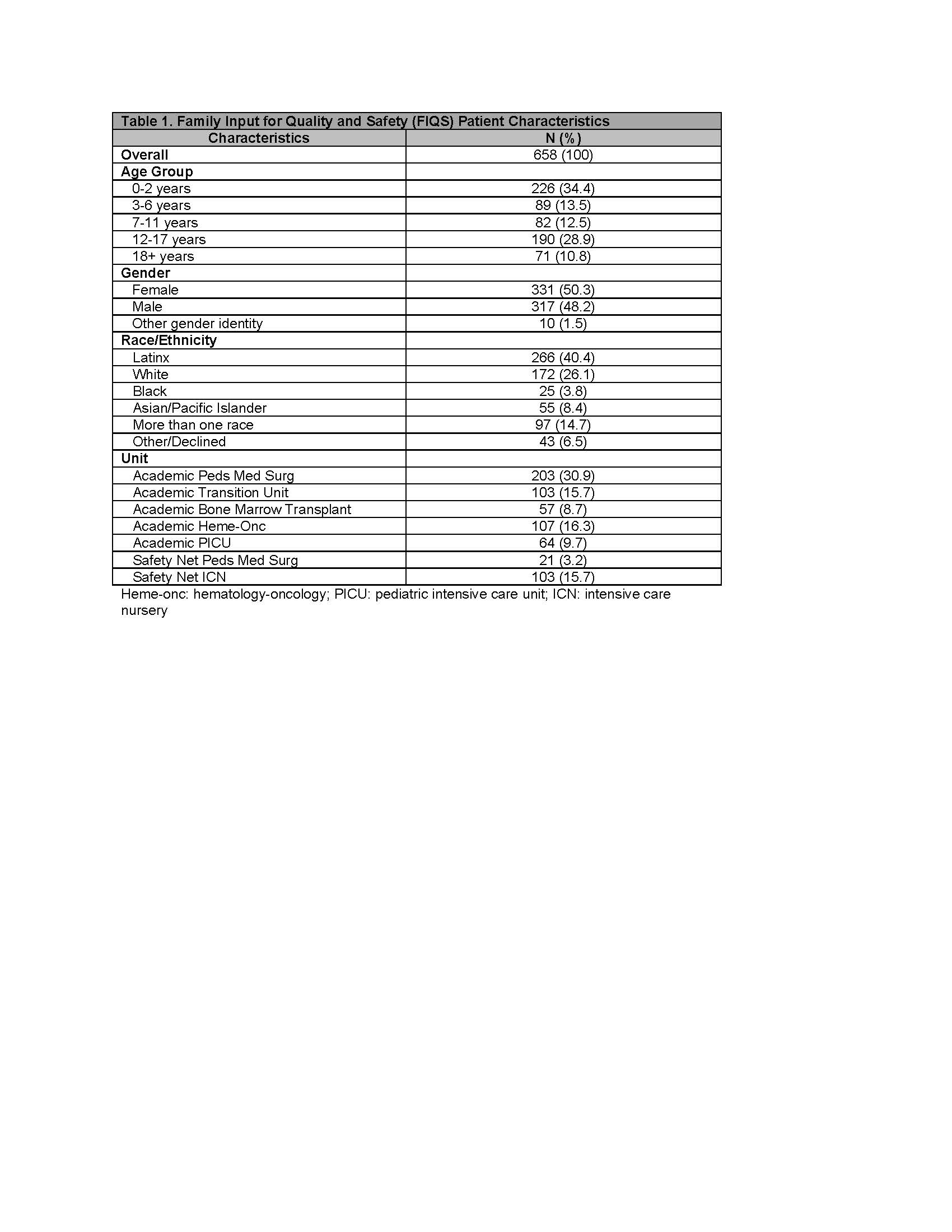
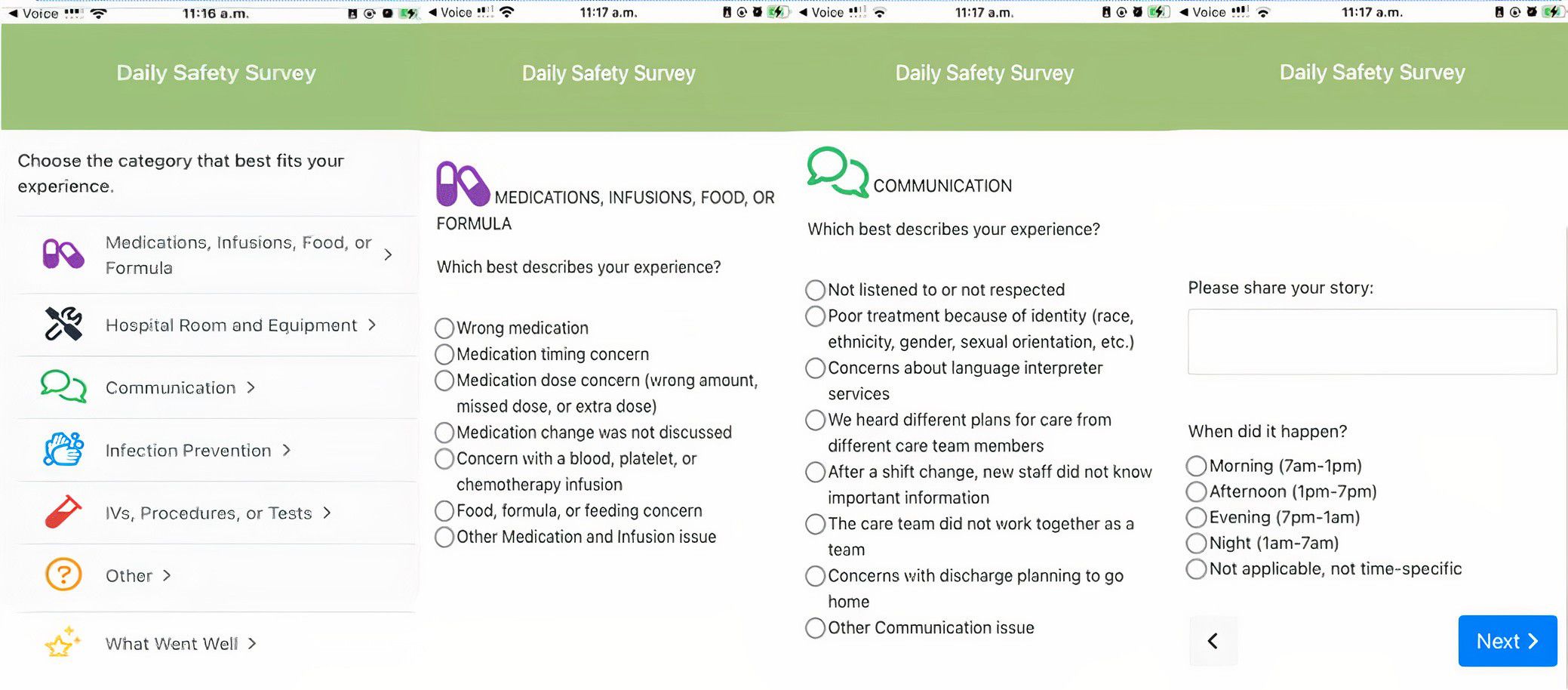
Adverse patient safety event rates remain stubbornly high in hospitals. Evidence suggests that family member and patient safety observations are clinically meaningful. To test a standardized approach to collecting these observations in the inpatient setting, we created the Family Input for Quality and Safety (FIQS) tool, a mobile phone interface (Figure 1). Based on patient and caregiver feedback, the tool includes positive valence reporting--events that enhance safety. In a pilot period, we found variation by race and ethnicity in reporting overall, but little is known about differential reporting by positive and negative (constructive) valence or whether interventions to increase positive reports might address disparities.
Objective:
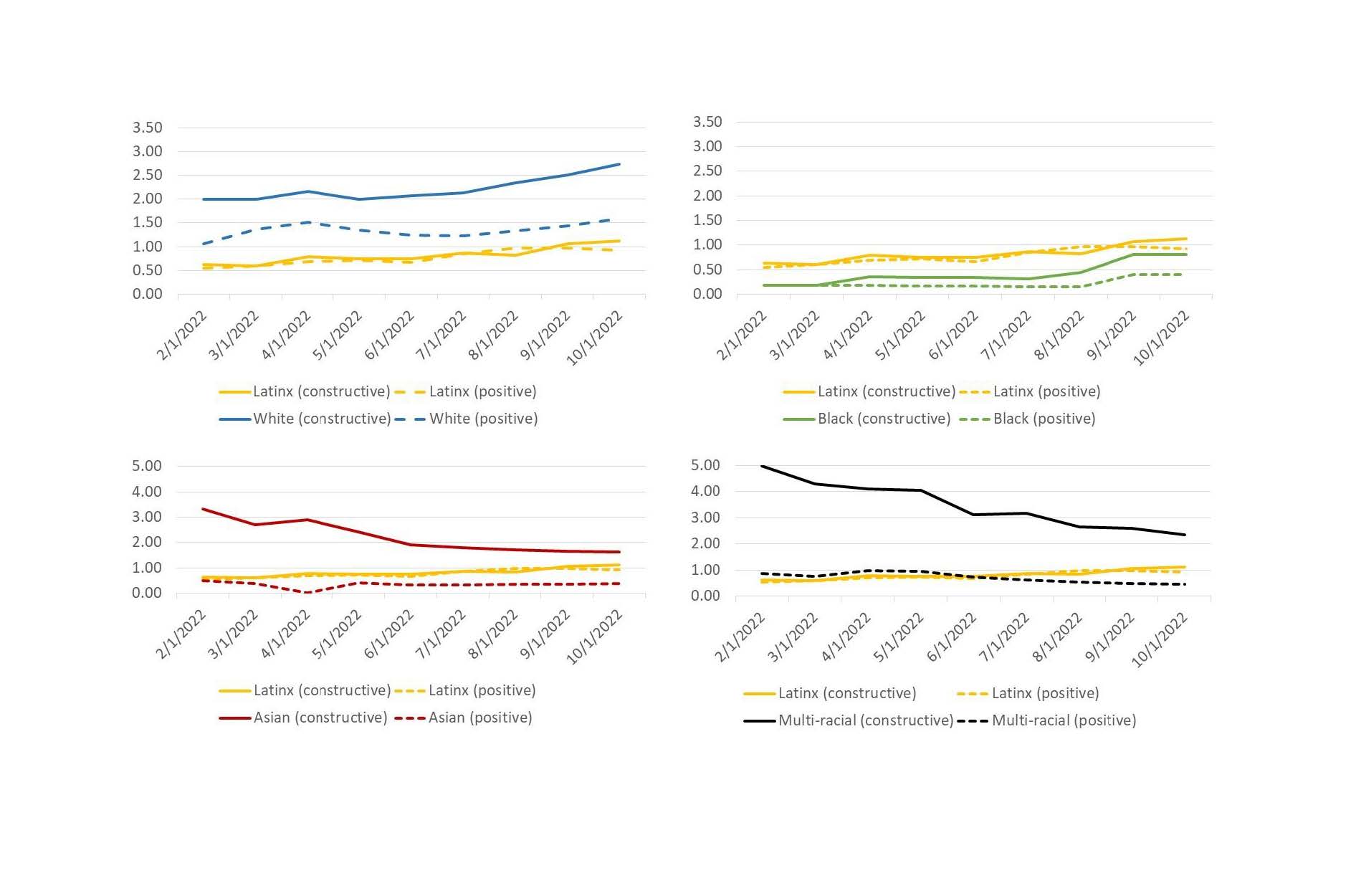
To improve the rate of patient and caregiver FIQS reports and to assess differences in positive and negative observation reporting rates by race and ethnicity.
Design/Methods: Participants (family members of admitted patients or patients 13+ years) were from multiple units in two hospitals (academic and safety net) 8/2021-10/2022. Unit leadership participated in a monthly collaborative 2/22-10/22, discussing data and approaches to improve engagement. We made 2 iterative tests of change (in June and August). Changes were based on family and patient advisory councils’ input and a literature review, indicating that encouraging all comments (negative AND positive) during recruitment and in the tool may increase reporting. We calculated the number of FIQS reports/100 patient-days and created run charts to assess changes in reporting over time by race/ethnicity.
Results: Participants (N=675) were associated with 658 pediatric patients (Table 1), and were mothers (n=446, 66%), fathers (n=117, 17%), and patients (n=87, 13%). Reporting rates differed substantially by race and ethnicity; trajectories changed over time, though slopes did not change with the tests of change. Latinx participants was the only group with similar rates of positive and negative safety observations, with all other groups with higher rates of negative observations (Figure 2).
Conclusion(s): Differences in reporting by race and ethnicity suggest differential willingness to engage with negative (or constructive) reporting. Prior evidence suggests that caregivers and patients may be reluctant to report on safety due to concerns of negative care repercussions. Our findings suggest that differences in cultural or personal preference may drive positive event reporting and indicate that interventions emphasizing the value of positive comments may have differential effects in different populations.