Quality Improvement/Patient Safety: Primary & Subspecialty Outpatient Quality Improvement
QI 6: Primary & Subspecialty Outpatient QI Group 1
256 - Improving Care of Childhood Obesity at a Community-Based Clinic: A Better Management Initiative through Quality Improvement (QI for BMI)
Publication Number: 256.452

P. Zhen Chan, MD MBA (he/him/his)
PGY-3
NewYork-Presbyterian Komansky Children’s Hospital
Weill Cornell Medicine
New York, New York, United States
Presenting Author(s)
Background: Childhood obesity affects 1 in 5 children in the United States, with the highest prevalence in Hispanic and non-Hispanic Black children. The American Academy of Pediatrics (AAP) endorses the 2007 Expert Committee Recommendations Regarding the Prevention, Assessment, and Treatment of Child and Adolescent Overweight and Obesity. The implementation of these guidelines varies in our primary care clinic.
Objective:
By July 2024, for patients aged 12-19 with BMI ≥ 95th percentile, our resident-led QI team aims to improve compliance with AAP practice recommendations to 90%. We define compliance as ordering recommended labs, adding diagnosis of obesity to a patient’s problem list, providing counseling, and scheduling follow-up appointments. While we successfully improved rates of recommending sooner follow-up appointments, appointment attendance remained unchanged. More recent interventions are not as of yet reflected in the current data. Our next steps will assess family socioeconomic and cultural factors that may play a role in accessing care and perceiving the need for follow-up appointments regarding obesity management.
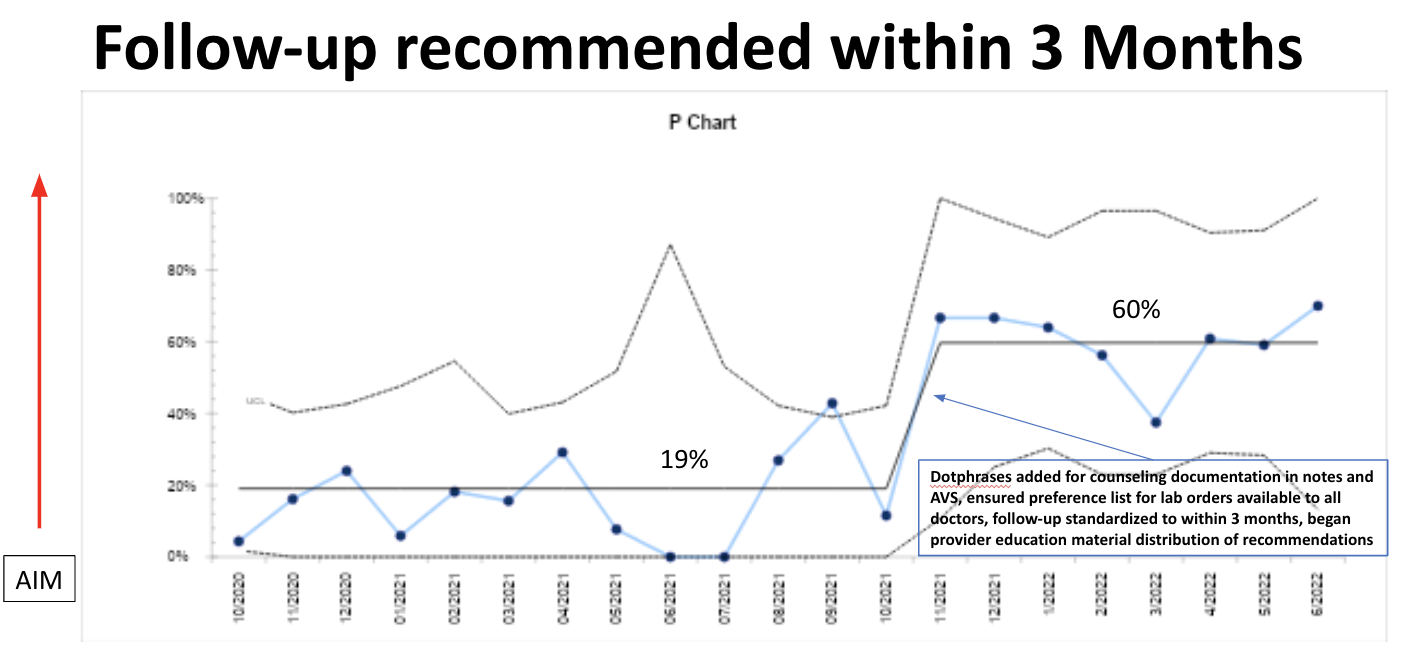
Design/Methods: In this observational time series performed at our primary care clinic affiliated with a tertiary academic medical center, residents used the model for improvement to test interventions designed to improve compliance with obesity guidelines (Figure 1). All patients with BMI ≥ 95% aged 12-19 were included. Process measures included recommended labs ordered or resulted within 2 years, obesity diagnosis added to problem list, counseling documented, 3-month or sooner follow-up recommended, follow-ups attended within 3 months, as well as any follow-ups attended prior to the next well visit were our outcome measures. We used monthly average PHQ-9 scores as a balancing measure considering the social stigma and mental health effects weight may cause. Data analysis was performed using statistical process control charts. API rules were applied to detect special cause variation.
Results: Between October 2020 and June 2022, we reviewed 417 charts. Rate of ordering recommended labs and adding obesity diagnosis to the problem list was high at 93 and 92% respectively (Figure 2). There was a decrease in counseling documentation provided from 89 to 76%. We detected special cause variation in the 3-month follow-up recommendation rates with an increase from 19% to 60% (Figure 3). However, attendance at recommended follow-ups within 3 months remained low at 3%, and overall at 11% before the next well visit. There was no change in PHQ-9 scores (balancing measure).
Conclusion(s): 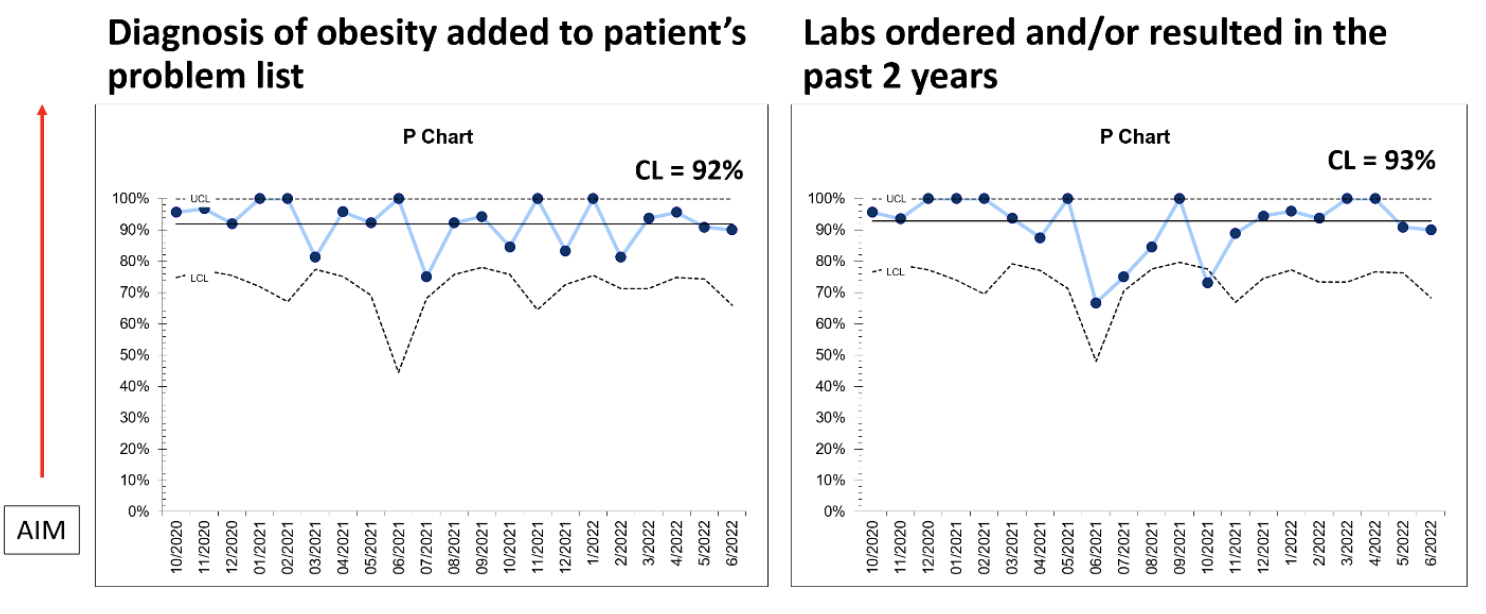
.png)
