Quality Improvement/Patient Safety: Primary & Subspecialty Outpatient Quality Improvement
QI 6: Primary & Subspecialty Outpatient QI Group 1
255 - An Innovative Medical-Dental Collaboration to Address Barriers to Pediatric Preventive Dental Care Among Medicaid-enrolled Children
Publication Number: 255.452

Jessica Weisz, MD (she/her/hers)
Assistant Professor
Children's National Health System
Washington, District of Columbia, United States
Presenting Author(s)
Background:
Tooth decay, the most common chronic disease in U.S. children, disproportionally affects low resourced communities leading to poor long-term health outcomes (Pregnancy and Early Childhood, n.d.). In DC in 2020, 38.5% of Medicaid patients aged 1-20 received preventative dental care (Percentage of Eligibles Who Received Preventive Dental Services: Ages 1 to 20 | Medicaid, n.d.).
Children’s Dental Health Project. The State of Dental Health: Pregnancy and Early Childhood.
State Health System Performance. Percentage of Eligibles Who Received Preventive Dental Services | Medicaid.
Objective: Incorporate Community Dental Health Coordinator (CDHC) via American Dental Association (ADA) model to increase preventative dental visits in an outpatient academic pediatric practice (Grover, 2014).
Grover, Jane. August 2014. Community Dental Health Coordinator. ADA.
Design/Methods: The CDHC, who is reflective of the community served of primarily Black children and families, was implemented at two community sites using an iterative plan-do-study-act (PDSA) model. CDHC screened all patients between ages 2 and 18 years at their preventative well visits for dental needs. If family agreed to CDHC support, CDHC evaluated and addressed barriers to access for prior preventative dental care and made family an appointment for dental cleaning with a community dental provider. CDHC followed up with families via phone to verify if family attended the appointment and addressed new barriers if needed. All patients received at least one phone call for follow up.
Results:
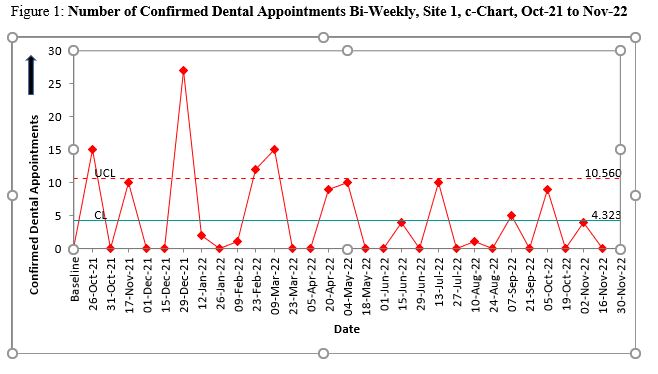
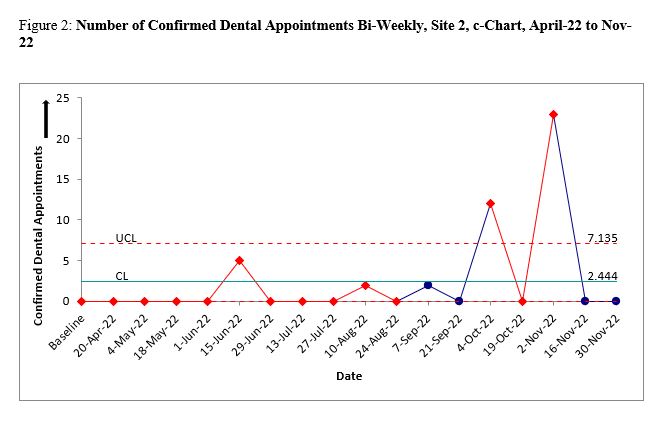
At Site 1, 432 of 1369 (31.5%) patients accepted CDHC support and 399 dental appointments were made. Of those, 218 patients (54.6%) were reached for follow up and 119 patients went to dental appointments (29.8%). At site 2, 177 of 794 (22.9%) patients accepted CDHC support and 175 dental appointments were made. Of those, 72 patients (41.1%) were reached for follow up and 44 patients went to dental appointments (25.1%).
Conclusion(s):
Patient uptake of CDHC intervention and dental appointment attendance was less than expected based on the need presumed by published Medicaid rates of preventative oral health care. PDSA cycles did not sustain patient engagement. Phone-follow up was difficult method to track dental appointment attendance. Families often missed scheduled appointments. Few dental clinics provide age-appropriate dental care in the same neighborhood as the medical home. To optimize the CDHC process, focus groups of patients and providers were conducted. Analysis will inform future PDSA cycles to improve the role of the CDHC and future interventions.