Neonatal/Infant Resuscitation
Neonatal/Infant Resuscitation 4
698 - Wrist vs ear pulse oximetry for neonates during resuscitation: a randomised controlled trial
Publication Number: 698.445
- KN
Kirti Naranje, MD (she/her/hers)
Additional Professor and Head, Neonatology
Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow
Lucknow, Uttar Pradesh, India
Presenting Author(s)
Background:
Excessive oxygen during neonatal resuscitation in delivery room is associated with various short and long-term morbidities. Pulse oximetry remains the essential tool in determining infant`s oxygenation and titration of oxygen delivery. The updated Neonatal Resuscitation Program 2021 advocated the use of pulse oximetry during resuscitation when there is a need for positive pressure ventilation or supplemental oxygen. For pulse oximetry to be useful in delivery room, the sensor has to be quickly applied to a suitable site on infant and then should be able to rapidly obtain a reliable signal. However, this can be quite challenging due to poor peripheral perfusion in first few minutes of life, effects of transitional circulation, motion artifact, presence of vernix and skin edema. This study explores the possibility of right ear as an alternate preductal site for rapid signal detection during newborn resuscitation in delivery room.
Objective:
To compare time taken for reliable oxygen saturation (SpO2) from the time of application of sensor at ear lobe vs right wrist during neonatal resuscitation.
Design/Methods:
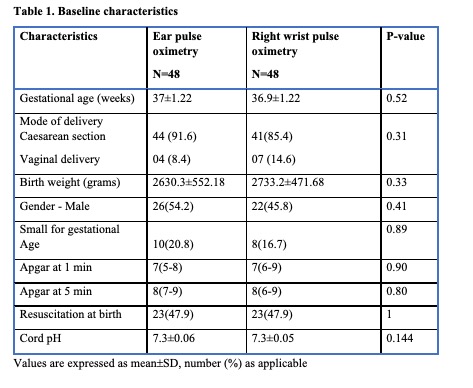
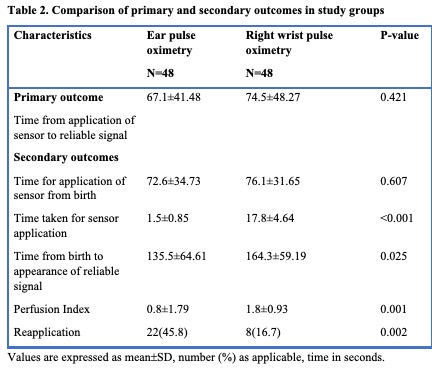
This trial was conducted in a level III neonatal unit over a 6-month period (July2022-December2022). All mothers ³34 weeks gestation with imminent or elective delivery were potentially eligible for enrollment. Pregnancies with antenatally diagnosed major congenital malformations, stillbirths, multiple gestation and severe birth asphyxia were excluded. Sensor to oximeter first(STOF) method was used in both groups. The primary outcome was time to reliable display of SpO2 and heart rate (HR) from the time of application of sensor to infant. Time from birth to application, time taken for sensor application, total time taken from birth to reliable signal, perfusion index and number of reapplication were secondary outcomes.
Results:
Ninety six neonates were randomised with 48 each in ear and wrist group. The mean time(seconds) to reliable display of signal from application was similar in both groups (67.1±41.4 vs 74.5±48.2 P=0.42). Amongst the secondary outcomes, time for sensor application(1.5±0.8 vs 17.8±4.6 P< 0.001) and overall time from birth to appearance of reliable signal(135.5±64.6 vs 164.3±59.1 P <0.02) were significantly lower in ear group. However, perfusion index was significantly lower(0.8±1.7 vs 1.8±0.9 P <0.001) and neonates requiring reapplication were higher in ear group[22 (45.8%) vs 8 (16.7%) P< 0.002].
Conclusion(s):
Both ear and right wrist pulse oximetry detected reliable SpO2 and heart rate in comparable time in delivery room setting.