Pulmonology
Pulmonology
174 - Spirometry in a Longitudinal Pediatric Population Pre- and Post COVID-19 infection
Publication Number: 174.449
- JH
Julia Harris, B.S. (she/her/hers)
Research Associate
Oregon Health & Science University School of Medicine
Portland, Oregon, United States
Presenting Author(s)
Background:
As of December 2022, over 15 million children have tested positive for COVID-19. Little is known about how this novel virus may impact long term health outcomes in children, particularly respiratory health of children exposed to in-utero and postnatal cigarette smoke. At this time there is no literature on spirometry pre and post COVID-19 infection in a pediatric population.
Objective:
To compare forced expiratory flows (FEFs) pre and post COVID-19 infection in a longitudinal cohort of children born to pregnant smokers. The occurrence of wheeze was also compared.
Design/Methods:
We identified children with a diagnosis of COVID-19 between 2/2020 to 9/2022 from a cohort of 213 children (age 5-8 years) being followed longitudinally from a randomized controlled trial (RCT) of vitamin C supplementation versus placebo to pregnant smokers. These children are studied with yearly spirometry and quarterly standardized respiratory questionnaires. As of June 2020, a yearly COVID-19 questionnaire was also administered. Spirometry was reviewed for adherence to ATS/ERS criteria. Wheeze was defined a priori as any of the following: parent report of wheeze, healthcare provider diagnosis of wheeze, or any bronchodilator or steroid use. Inclusion criteria: 1) Offspring of a pregnant smoker randomized in the above RCT; 2) Parent reported Yes to, “Has a healthcare provider ever told you that your child had, or likely had, COVID-19?” or a confirmed positive COVID-19 test via nasal swab; 3) Spirometry completed within one year pre- and post COVID-19 infection. The primary outcome was the comparison of FEFs (specifically FEF25-75 [FEF between 25% and 75% expired volume]) pre- and post COVID-19 infection. The occurrence of wheeze in the 1 year pre- and post COVID-19 diagnosis (yes versus no) was also compared.
Results:
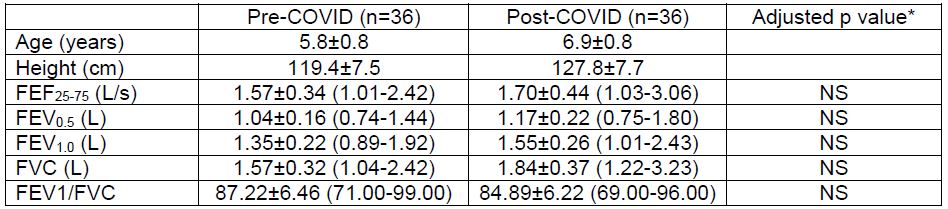
36 children met the inclusion criteria (64% white non-Hispanic; 47% male; 69% living with a smoking primary caregiver at the time of the pre-COVID spirometry; 8% with the diagnosis of asthma prior to COVID-19. Median age at COVID-19 infection was 7.0 years (range 5.4-8.8 years). None of the children required hospitalization. There was no significant difference between the pre- and post- spirometry data (Table 1) after adjustment for sex, race, height, and age at testing. Four children had wheeze in the year prior to infection, compared to 11 in the year post COVID-19 infection.
Conclusion(s): The results in this subset of patients from an ongoing longitudinal cohort show no difference in spirometry/ FEF25-75 in children born to pregnant smokers when tested within one-year pre and post COVID-19 infection.