Back
Background: The Niños Primeros en Salud (NPS) clinic in the rural town of Consuelo, Dominican Republic (DR) offers comprehensive pediatric care to over 600 children ages 0-5 years in 12 neighborhoods, concentrating on 5 key pillars of health: breastfeeding, immunizations, anemia, nutrition, and deworming as per WHO guidelines. The program also has a strong focus on community health through home visits, health education for families, and biannual deworming campaigns led by the nursing team and community health promoters.
Objective: To use quality improvement (QI) approaches to enhance pediatric care at the NPS clinic.
Design/Methods: The clinic team sets annual goals for each pillar. Patient medical record data corresponding to the pillars is digitized and updated in an electronic database after each patient visit. After each calendar month, data are summarized by pillar and analyzed using STATA. Data are then reviewed by the clinical team and a monthly Plan Do Study Act (PDSA) cycle is used for continuous improvement of patient care.
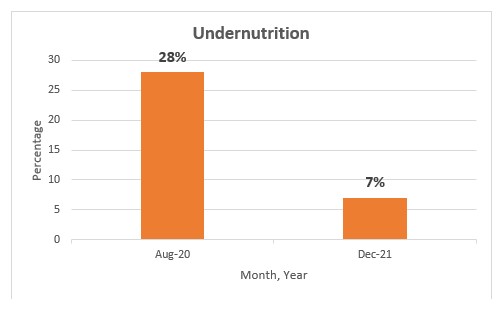
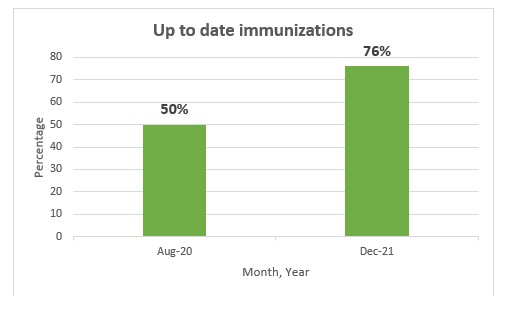
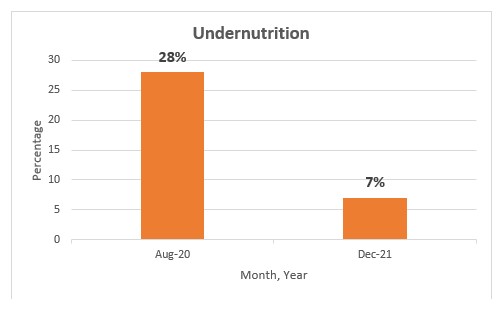
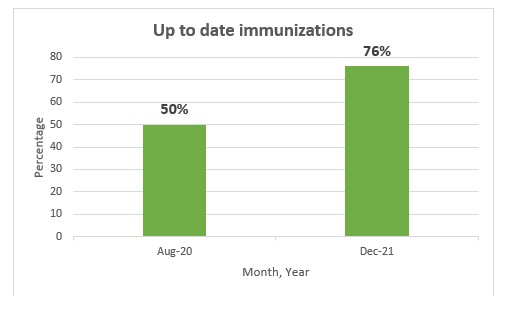
Results: In a cohort of 532 children over a 16-month period, we saw the following improvements: deworming of eligible children (2-5 years old) increased from 76% to 96%; a CBC completed at 15 months of age increased from 66% to 91% of patients; undernutrition decreased from 28% to 7%; up-to-date immunizations increased from 50% to 76% (Figures 1-3). Breastfeeding was the only pillar to see a partial negative change over the same period, with breastfeeding initiation in the first week of life decreasing from 77% to 65%, but the proportion of mothers who continued breastfeeding until at least 4 months increased from 53% to 81%. Data informed both educational activities and a discussion with the public health authorities over immunization shortages which was rectified. The clinical team remained engaged and increasingly proactive over the quality improvement period.
Conclusion(s): During this process we added overweight status as part of the healthy nutrition pillar as the team noticed overnutrition as an emerging problem and the clinic served an additional 4 neighborhoods. The PDSA approach facilitated steady improvements in 4 pillars, with only a reduction in breastfeeding initiation noticed. The team looks forward to ongoing QI in the years ahead and sharing the process with regional and national public health leaders with the hope of advancing child health in the DR.
.jpg)
Global Neonatal & Children's Health
Global Neonatal & Children's Health 3
545 - Using quality improvement (QI) to advance preventive child health in a rural clinic in the Dominican Republic
Monday, May 1, 2023
9:30 AM – 11:30 AM ET
Poster Number: 545
Publication Number: 545.409
Publication Number: 545.409
Anabel Fernandez, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Krupal Rana, Children's Hospital of Phildadelphia, Philadelphia, PA, United States; Bernard Caines, NIños Primero en Salud, Consuelo, San Pedro De Macoris, Dominican Republic; Ramona Cordero, Niños Primeros en Salud, Consuelo, San Pedro De Macoris, Dominican Republic; Ingrid Japa, Universidad Central del Este School of Medicine, San Pedro de Macoris, San Pedro De Macoris, Dominican Republic; Angie E. Alvarez, Niños primeros en salud, SAN PEDRO de Macoris, San Pedro De Macoris, Dominican Republic; Ivelisse Tavarez, Niños Primeros en Salud, Consuelo, San Pedro De Macoris, Dominican Republic; Andrew P. Steenhoff, Children's Hospital of Philadelphia & UPenn, Philadelphia, PA, United States

Anabel Fernandez, MPH (she/her/hers)
Global Health Program Manager
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: The Niños Primeros en Salud (NPS) clinic in the rural town of Consuelo, Dominican Republic (DR) offers comprehensive pediatric care to over 600 children ages 0-5 years in 12 neighborhoods, concentrating on 5 key pillars of health: breastfeeding, immunizations, anemia, nutrition, and deworming as per WHO guidelines. The program also has a strong focus on community health through home visits, health education for families, and biannual deworming campaigns led by the nursing team and community health promoters.
Objective: To use quality improvement (QI) approaches to enhance pediatric care at the NPS clinic.
Design/Methods: The clinic team sets annual goals for each pillar. Patient medical record data corresponding to the pillars is digitized and updated in an electronic database after each patient visit. After each calendar month, data are summarized by pillar and analyzed using STATA. Data are then reviewed by the clinical team and a monthly Plan Do Study Act (PDSA) cycle is used for continuous improvement of patient care.
Results: In a cohort of 532 children over a 16-month period, we saw the following improvements: deworming of eligible children (2-5 years old) increased from 76% to 96%; a CBC completed at 15 months of age increased from 66% to 91% of patients; undernutrition decreased from 28% to 7%; up-to-date immunizations increased from 50% to 76% (Figures 1-3). Breastfeeding was the only pillar to see a partial negative change over the same period, with breastfeeding initiation in the first week of life decreasing from 77% to 65%, but the proportion of mothers who continued breastfeeding until at least 4 months increased from 53% to 81%. Data informed both educational activities and a discussion with the public health authorities over immunization shortages which was rectified. The clinical team remained engaged and increasingly proactive over the quality improvement period.
Conclusion(s): During this process we added overweight status as part of the healthy nutrition pillar as the team noticed overnutrition as an emerging problem and the clinic served an additional 4 neighborhoods. The PDSA approach facilitated steady improvements in 4 pillars, with only a reduction in breastfeeding initiation noticed. The team looks forward to ongoing QI in the years ahead and sharing the process with regional and national public health leaders with the hope of advancing child health in the DR.
.jpg)