Neonatal Pulmonology
Neonatal Pulmonology 5: NICU Practices
156 - Surfactant Delivery via Thin Catheter in Preterm Infants with Respiratory Distress Syndrome: A Systematic Review and Meta-Analysis
Publication Number: 156.437
- TY
Telford Yeung, MD PhD
Neonatologist
University of Windsor
Windsor, Ontario, Canada
Presenting Author(s)
Background:
Surfactant administration via a thin catheter is an alternative to surfactant administration post endotracheal intubation in preterm infants with respiratory distress syndrome (RDS); however, the benefits particularly in extremely low gestational age neonates (ELGANs: less than 28 weeks’ gestation) and the neurodevelopmental outcomes remain unclear.
Objective:
To systematically review and meta-analyze the efficacy and safety of surfactant administration via thin catheter in preterm infants with RDS.
Design/Methods:
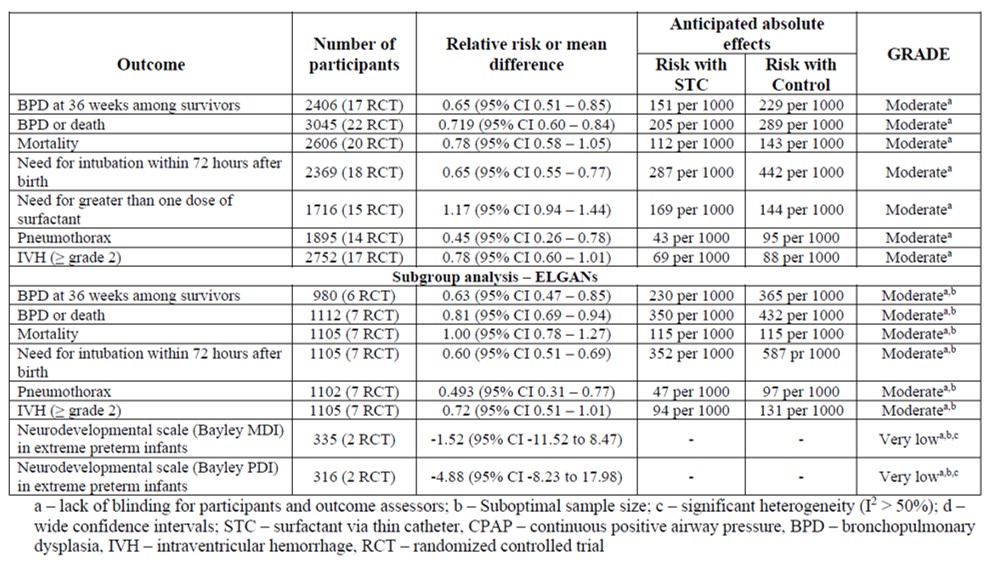
Medical databases including those from China were searched until December 2022 for randomized controlled trials (RCTs) assessing surfactant administration via thin catheter (STC) versus intubation for surfactant with early or delayed extubation or nasal continuous positive airway pressure (nCPAP) in preterm infants with RDS. The primary outcome was bronchopulmonary dysplasia (BPD) in survivors. Secondary outcomes included BPD or death, mortality, need for intubation within 72 hours, need for more than one dose of surfactant, pneumothorax, intraventricular hemorrhage (IVH ≥ grade 2) and neurodevelopmental outcomes. Subgroup analysis was conducted in ELGANs. The Cochrane risk of bias (ROB) tool was used to assess bias for included RCTs. A random-effects model was used for meta-analyses, and evidence was rated according to GRADE.
Results:
Twenty-six RCTs of 3349 preterm infants were included. The majority of included studies had low ROB. STC significantly decreased the risk of BPD in survivors compared to controls [17 RCTs; N = 2406; relative risk (RR) = 0.65; 95% confidence interval (CI) 0.51 to 0.85; Risk difference (RD) = -0.05; 95% CI -0.90 to -0.01; NNTB = 13; GRADE: moderate]. Compared to controls, STC significantly decreased the incidence of BPD or death, need for intubation within 72 hours of birth and pneumothorax with no differences in other prespecified outcomes. Compared to controls, STC significantly decreased BPD in ELGANs [6 RCTs; N = 980; RR = 0.63; 95% CI 0.47 to 0.85; RD = -0.17 95% CI -0.30 to -0.03; NNTB = 7].
Conclusion(s): Compared to controls, STC is a more effective and equally safe method of surfactant delivery in preterm infants and in the ELGAN subpopulation. Adequately powered trials in ELGANs with a focus on long term neurodevelopmental outcomes are needed.