Quality Improvement/Patient Safety: Primary & Subspecialty Outpatient Quality Improvement
QI 6: Primary & Subspecialty Outpatient QI Group 1
260 - Improving Adherence to AAP & CDC Guidelines for the Care of Immigrant and Remigrant Children in a Pediatric Ambulatory Care Network
Publication Number: 260.452

Zachary Berlant, MD (he/him/his)
Resident
NewYork-Presbyterian Morgan Stanley Children's Hospital
New York, New York, United States
Presenting Author(s)
Background: In 2016, the AAP established recommendations to address the unique needs of immigrant children in pediatric primary care. As rates of children immigrating to the United States are increasing, there is a greater need to provide the appropriate care. A needs assessment at our institution found that rates of guideline adherence were low for most recommendations.
Objective: To use QI methodology to improve adherence to AAP and CDC recommendations for immigrant and remigrant children at an ambulatory, academic pediatric practice from a median of 24.5% to 49%.
Design/Methods:
This 1 year-long QI project utilized PDSA cycles involving education, electronic health record aids, and provider feedback, to increase the rate of providing the recommended care for immigrant and remigrant children in 1 adolescent and 4 general pediatric clinics (Fig 1, 2).
Children were identified as immigrating or remigrating if they were seeking care after living in another country for at least one year. Subjects ages 0-18 years-old were screened for inclusion based on receipt of a serum Quantiferon-TB Gold or TB skin test (TST), followed by chart review.
Provider compliance was defined as meeting (>50%) of the recommended care for guidelines that apply to all migrant children (Fig 3, Sec 1). The outcome measure of providing recommended screenings was tracked overtime with a run chart and compared to the baseline period (Fig 2). As a balancing measure, we tracked rates of appropriately managed abnormal labs.
Chi-square of homogeneity and Mann Whitney U tests were used to compare the rates of screening at baseline to rates during the QI project. Unadjusted and Mantel-Haenszel Odds ratios (MH ORs) were calculated for each recommendation (Fig 3).
Results: Compliance rates increased from median 24.5% to 59.5% (Fig 2). There was a difference in percent of new migrants (44 vs 71%, p < 0.05), between the baseline and QI implementation periods. There was no difference in sex, age, or percent of adolescents. MH ORs were increased for the majority of screenings and 4 individual screenings, however all had residual confounding (Fig 3). As the number of labs increased during the implementation period, all abnormal results (n=7/7) were appropriately triaged.
Conclusion(s): We outperformed our outcome goal to improve screening for immigrant and remigrant children. PDSA cycles rapidly resulted in improvement which was sustained over the implementation period. Ordersets, smartphrases, provider education and feedback were most impactful. Abnormal results from increased screenings were appropriately managed 100% of the time.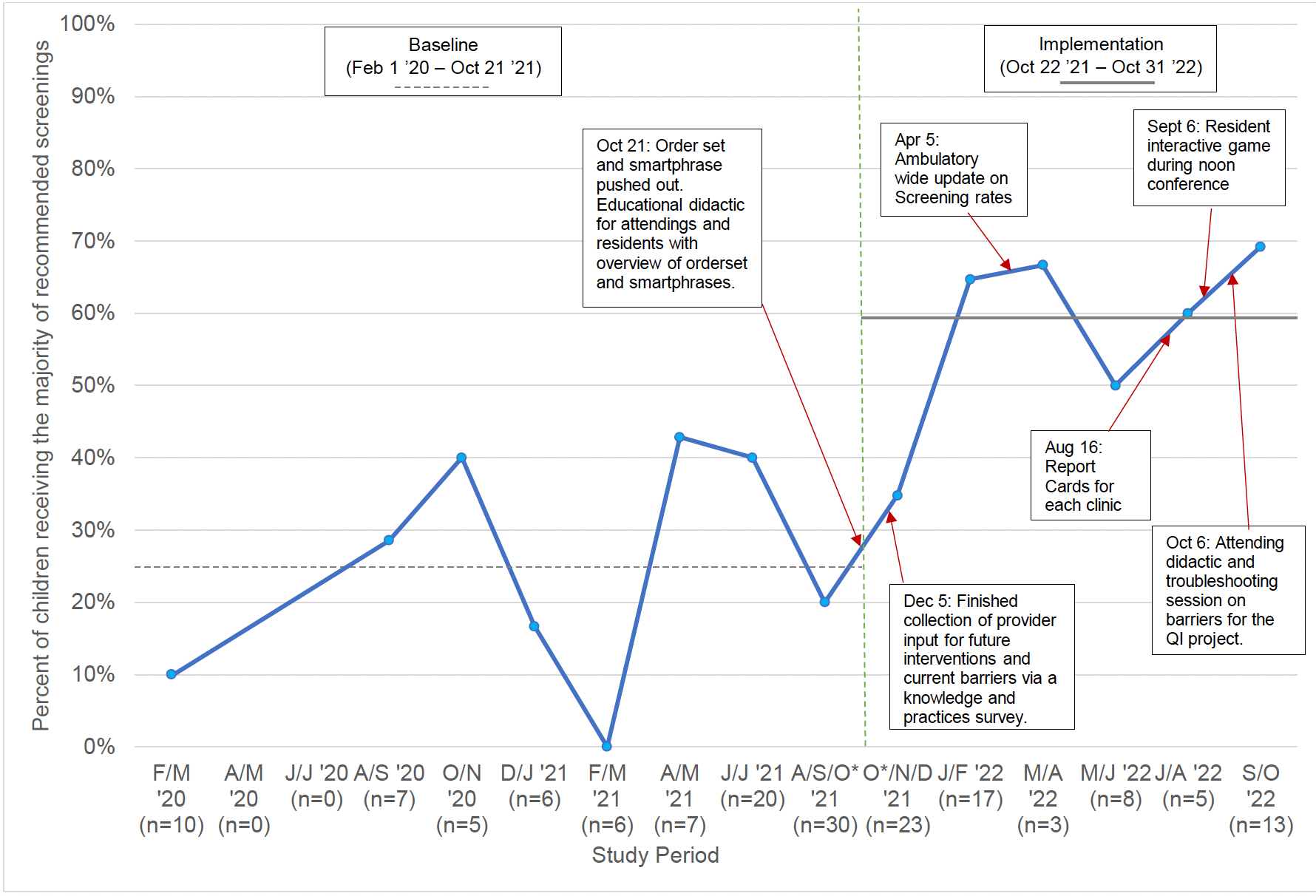
.png)
.png)
