Neonatal Quality Improvement
Neonatal Quality Improvement 7
214 - The Implementation Of A New Evidence-based Bundle For Reduction Of Central Line-Associated Bloodstream Infection (CLABSI) Incidence In A Tertiary Level NICU: A Prospective Study
Publication Number: 214.441

Gianluca Lista (he/him/his)
Chief Neonatologist
NICU, V.Buzzi Children's Hospital
V.Buzzi Children's Hospital, ASST-FBF-Sacco
milan, Lombardia, Italy
Presenting Author(s)
Background:
CLABSI is a significant cause of morbidity and mortality in NICUs. A bundle is a small, straightforward set of evidence-based practices proven to improve patient outcomes when performed collectively and reliably.
Objective:
to assess the impact of a new evidence-based bundle for central line insertion, dressing, and maintenance and the use of new materials on the rate of CLABSI in a tertiary-level NICU.
Design/Methods:
We performed a prospective, quality improvement (QI) study on all consecutive neonates (January 2021-August 2022) admitted to the NICU and receiving a central line. The bundle included use of: polyurethane catheters only, the RaSuVa (rapid superficial vein assessment) protocol to identify the most appropriate vein, 2% chlorhexidine solution in disposable pre-dosed applicators for disinfection, cyanoacrylate glue plus a sutureless device (Grip Lok) plus a Transparent Semipermeable Membranes (TSM) with High Moisture Vapor Transmission Rates (HMVTR) for medication and stabilisation of the exit site, needle-free connectors and alcohol-impregnated port-protectors to disinfect the catheter hubs. Study period was divided into quarters: Period 1 pre-intervention (old bundles and pre-existing materials), P2 intervention (bundle and new materials introduction), P3 post-intervention, and P4-P5 maintenance. Data from the 4 periods were analyzed and are still being collected after the study to verify sustainability. The main QI measure was the rate of CLABSI.
Results:
147 neonates for a total of 279 central venous catheters inserted and 2857 catheter days were analyzed. A total of 34 CLABSI were registered during the observation (overall CLABSI incidence: 12.01/1000 central line days (95% CI 8.3-16.7).
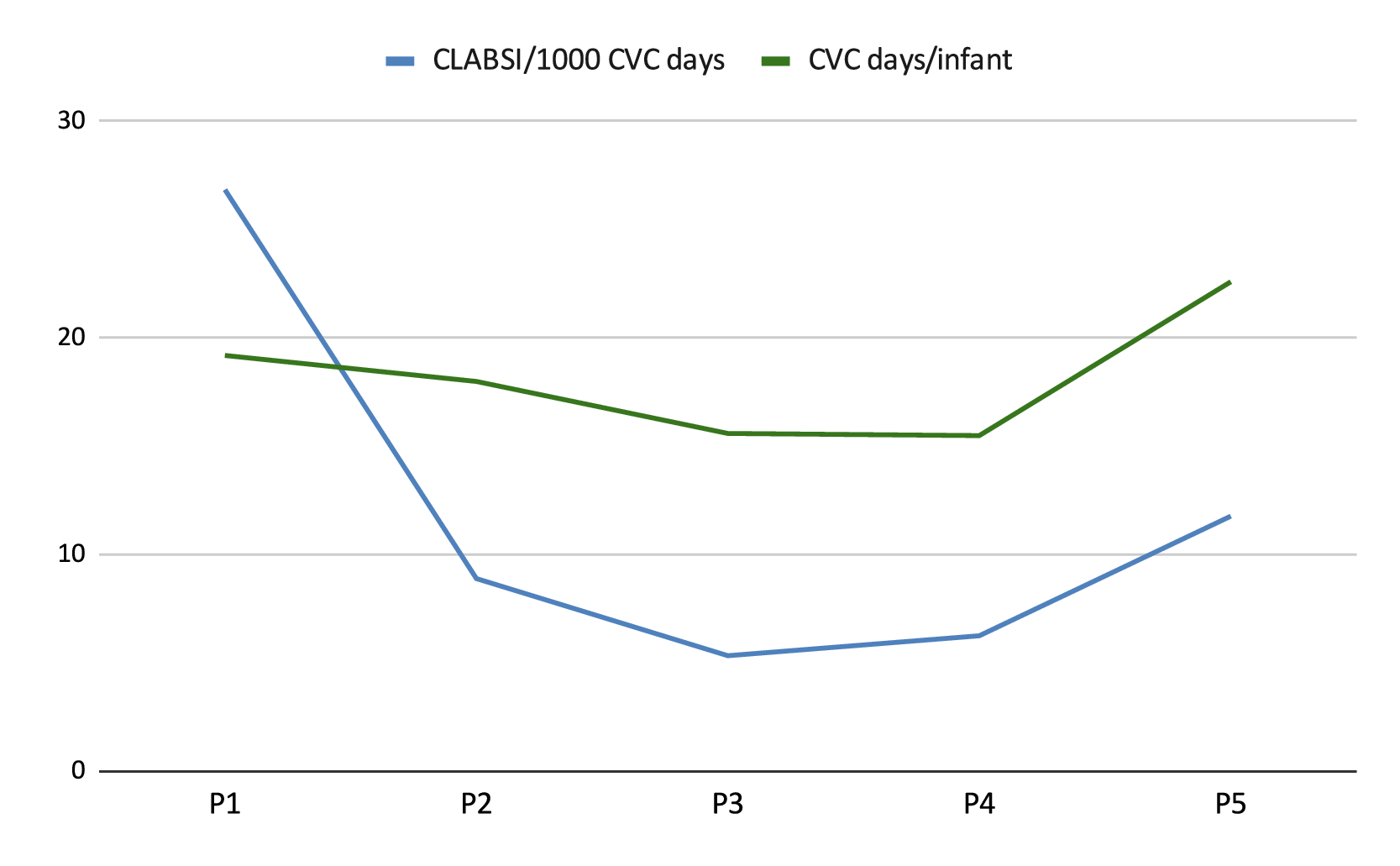
CLABSI incidence significantly decreased from P1 (26.85 CLABSIs per 1000 catheter days, 95%CI 15.4-43.2) to P2 (8.9/1000 CVC days, 95% CI 2.9-20.7) (p=0.02) to P3 (5.34/1000 CVC days, 95%CI 1.1-15.5) (p=0.004); it was 6.26/1000 CVC days (95%CI 1.3-18.2) in P4 and increased in P5 to 11.78 CLABSIs per 1000 CVC days (95%CI 4.5-22.7); both P4 and 5 still showed a significant reduction from the pre-intervention rate (p=0.01 and =0.0416, respectively). Fig 1.
Conclusion(s):
In our NICU population the the incidence of CLABSI promptly significantly decreased with the implementation of evidence based bundles. Maintenance period showed increasing CLABSI incidence, though still improved versus pre intervention period, possibly due to a lower adherence to the bundles after the first period, confirming the importance of constant updates and education.