Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 5: Surfactant and NIV 2
669 - Clinician Opinions on Nasal versus Oral Intubation in Infants with Bronchopulmonary Dysplasia
Publication Number: 669.443

Jessica L. Vitale, BS (she/her/hers)
Medical Student Research Intern
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background:
Nasal rather than oral endotracheal tube (ETT) placement may reduce accidental extubation and improve clinical outcomes during brief periods of mechanical ventilation. The optimal route of intubation in infants with bronchopulmonary dysplasia (BPD) who require prolonged invasive ventilation is uncertain.
Objective:
We surveyed clinicians who work in the neonatal intensive care unit (NICU) at a single quaternary referral center (~3% rate of nasal intubation) to understand their perceptions of the risks and benefits of nasal versus oral intubation in BPD.
Design/Methods:
Over a 2-week period in 2022, a 16-question survey was distributed to attending physicians (MD/DO), front-line clinicians (FLC), nurses (RN), physical/occupational therapists (PT/OT), and respiratory therapists (RT) who provide clinical care to infants with BPD. Clinicians' opinions were assessed via Likert scale (5-scale consolidated to 3-scale for analyses).
Results:
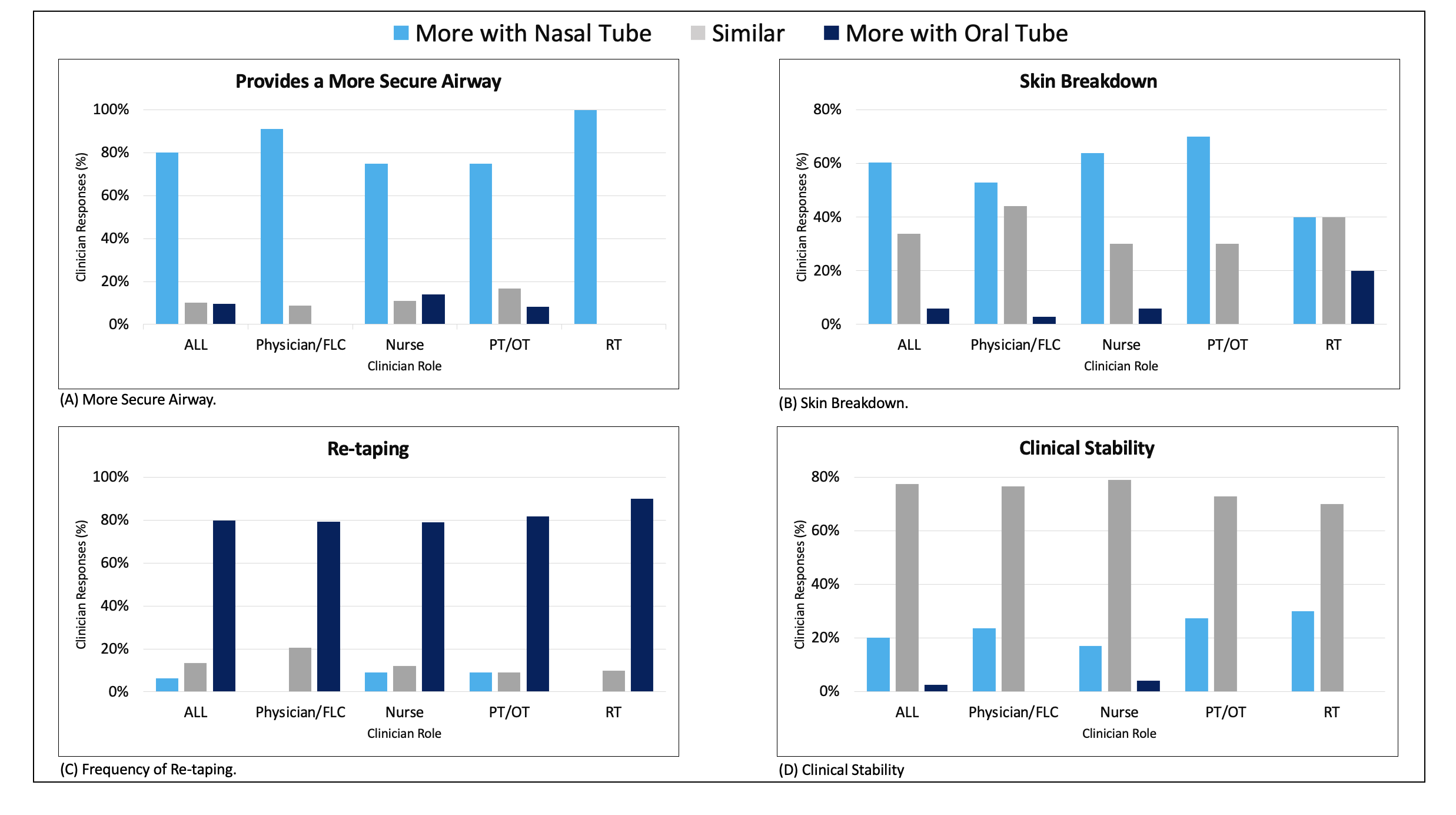
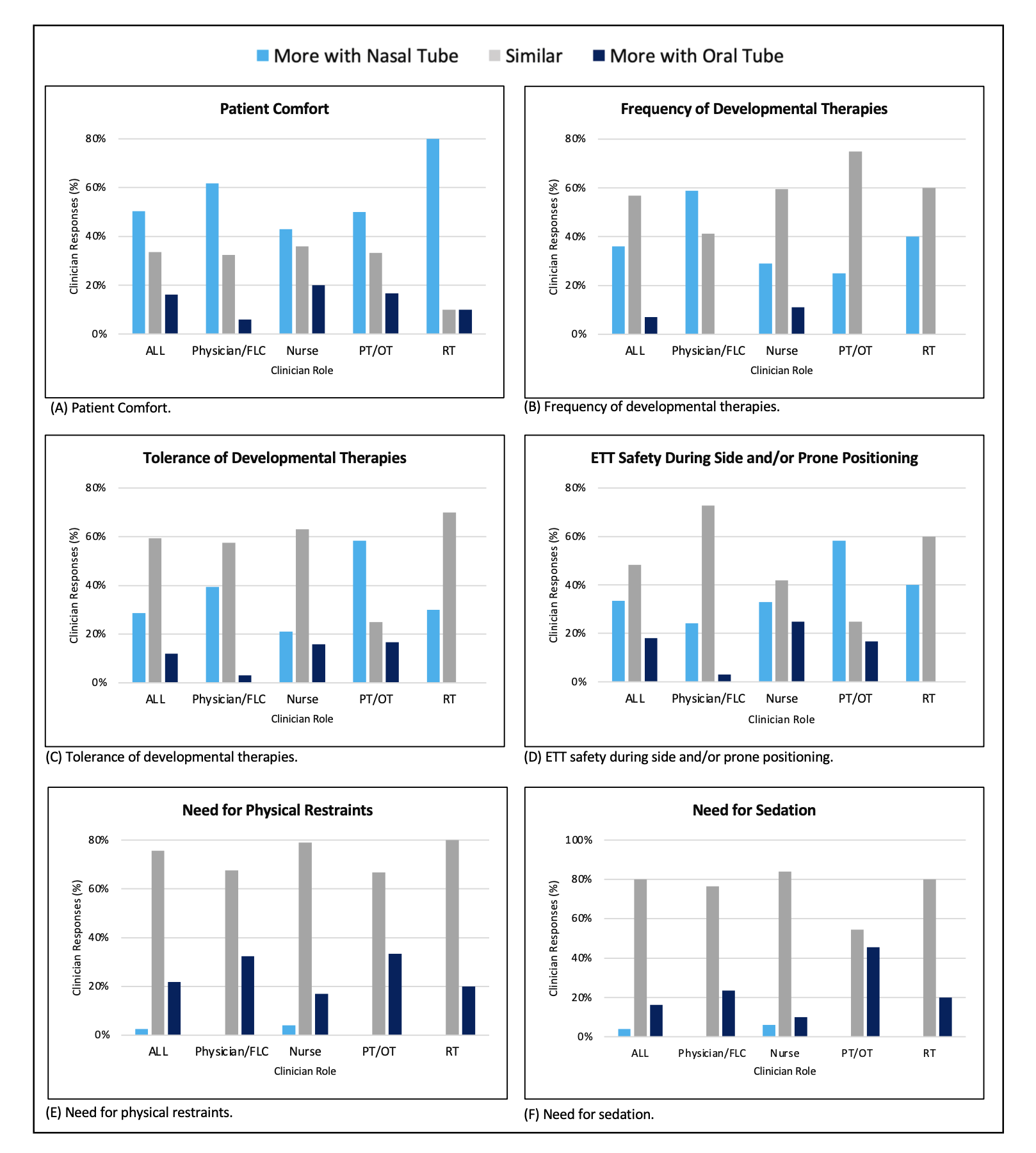
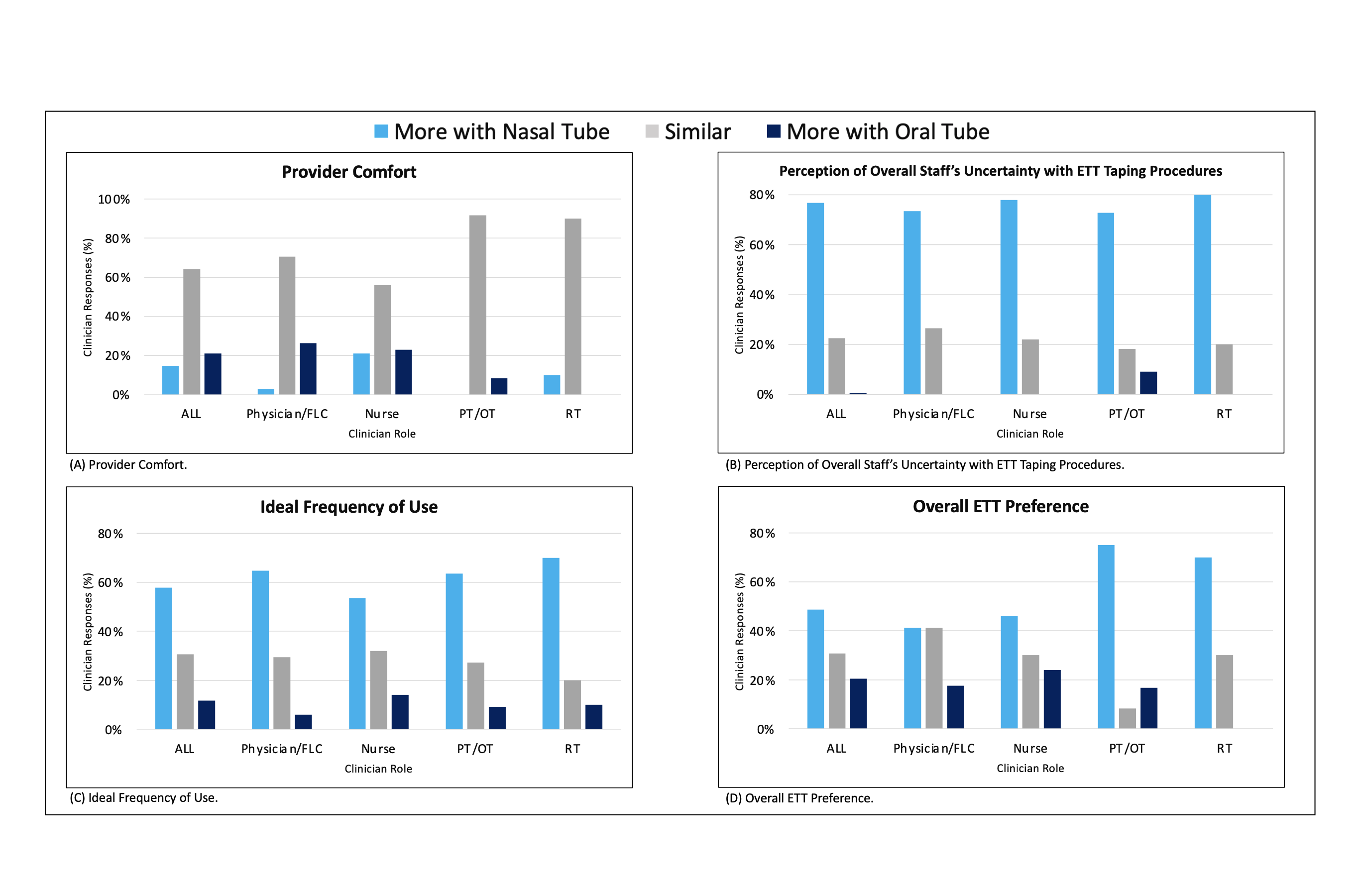
162 clinicians responded (response rates: MD/DOs 49%, FLCs 44%, RTs 90%, RNs 40%); data from 156 respondents who have cared for infants supported by nasal intubation were analyzed. The cohort consisted of 27 MD/DOs, 7 FLCs, 100 RNs, 12 PT/OTs and 10 RTs. The mean years of experience was 8.2 (SD: 8.7). The majority reported that nasal as compared to oral ETTs provide a more secure airway (80%) and require less frequent re-taping (80%) but may not result in differences in clinical stability (Fig 1). There was also concern that nasal ETTs may increase risk of skin breakdown (Fig 1B). PT/OTs indicated nasal ETTs improve patient tolerance of therapy, but this potential benefit was not endorsed by other clinician subtypes (Fig 2). Most respondents indicated that ETT location did not affect need for sedation or physical restraint in infants with BPD (Fig 2 E-F). With respect to clinician comfort, most (77%) indicated NICU staff were more certain with taping procedures for oral versus nasal ETTs (Fig 3B). Most clinicians (58%) favored more frequent use of nasal ETTs (Fig 3C). In total, 49% indicated an overall preference for nasal ETTs, 21% preferred oral ETTs, and 31% had no preference (Fig 3D). When stratified by role, PT/OTs (75%) and RTs (70%) were the most likely clinicians to prefer nasal ETTs.
Conclusion(s):
Opinions on nasal versus oral intubation in preterm infants with BPD varied. However, a plurality preferred nasal compared to oral intubation for infants with BPD who require prolonged mechanical ventilation. These data support unbiased evaluation of nasal intubation as a possible means to improve clinical outcomes in BPD.