Emergency Medicine: All Areas
Emergency Medicine 15
398 - Point of Care Electrolyte Testing: "Lyte"ning the Visits in Urban Pediatric Emergency Center
Publication Number: 398.406

Arooma Ismail, MBBS (she/her/hers)
PGY-5
Beaumont Hospital
Icahn School of Medicine at Mount Sinai- Elmhurst Hospital Center
Royal Oak, Michigan, United States
Presenting Author(s)
Background: Point of care testing (POCT) is well established for rapid results on glucose, blood gas and electrolytes. POCT has been studied extensively in adults but studies in pediatric patients are not as common, especially for non-diabetic care.
Objective: The primary objective of this study is to describe the utilization of POCT for electrolytes in non-diabetic pediatric patients in the ED; comparing their use related to blood serum electrolyte testing and potential IV fluids ordered and impact on length of stay (LOS).
Design/Methods:
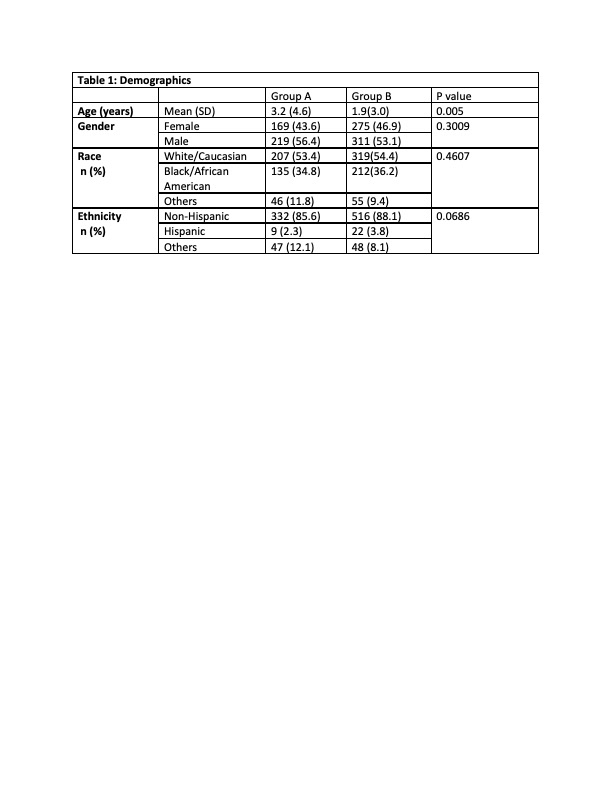
Retrospective chart review of all pediatric ED visits, age 0 months to 17 years, that had POCT electrolytes ordered between 3/1/2017 to 2/29/2020 (pre-COVID) in the pediatric ED. Exclusion criteria was anyone with diabetes. Data extracted were patient demographics, chief complaint, BMP/CMP order, IV fluids order, ED length of stay, final disposition, and diagnosis.
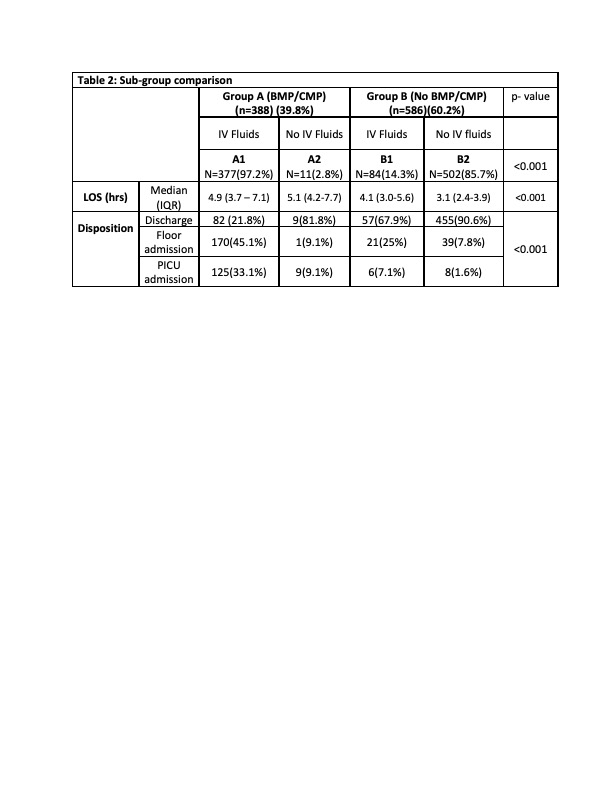
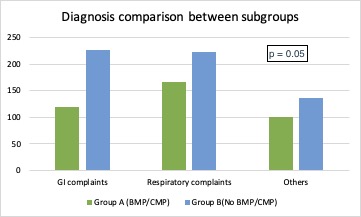
Results: 974 total children had POCT electrolytes with a median age of 1 year (IQR 0-3). Overall, 45.6% patients were female, and 37.6 % were admitted to the hospital. Of 974 patients, 39.8% had BMP/CMP (defined as group A) and 60.2% did not(defined as group B). IV fluid use was 97.2% patients from group A and 14.3 % patients from group B. The median length of stay was 4.9 hrs (IQR 3.7-7.1) in group A and 3.2 hrs (IQR 2.5-4.2) in group B. Disposition differences were large (p< 0.001), with 23.4% of patients discharged and 32.5 % admitted to ICU from group A, and 87.4% of patients discharged and 2.4% admitted to ICU from group B. The numbers of patients in different categories of the disposition diagnosis were not significantly different between the the groups. Data was analyzed using Chi-Square test for comparing rates, Brown-Mood test for comparing median and Wilcoxon test for comparing means among the groups. The level of significance was set at < 0.05.
Conclusion(s):
The findings of this study suggest that POCT results play a valuable role in ED decision making for children. The majority of patients did not have serum electrolytes after the POCT test and were discharged from the ED in shorter time. Sub-group analysis has shown significant difference in rate of IV fluids order, length of stay and disposition. It is likely that the POCT impacts care positively with shorter LOS and less blood draws needed as seen in this study. This will need further prospective investigation. This information can help to create a future clinical pathway for POCT guidelines, and those guidelines can help decreasing the need for central lab testing and IV fluids thus shortening the length of stay.