Emergency Medicine: All Areas
Emergency Medicine 14
379 - Epidemiology of Emergency Department Visits for Children with Complex Cardiovascular Disease
Publication Number: 379.405
- ZA
Zaynah Abid, MD, MPH (she/her/hers)
Pediatric Emergency Medicine Fellow
Columbia University Vagelos College of Physicians and Surgeons
New York, New York, United States
Presenting Author(s)
Background:
There is a paucity of data regarding the prevalence of emergency department (ED) visits, reasons for ED presentation and outcomes of children with complex cardiovascular disease (CVD).
Objective:
To understand the epidemiology of children with complex CVD presenting to pediatric EDs and identify factors associated with admission.
Design/Methods:
Using the Pediatric Health Information System (PHIS), we performed a retrospective analysis of encounters of children < 17 years old with complex CVD presenting to an ED from 46 U.S. children’s hospitals between 2016 and 2021. Patients were included if they had a cardiovascular complex chronic condition (CCC), defined by ICD-10 diagnosis and procedure codes. Based upon the type of CVD, we assessed the primary visit diagnosis, diagnostic testing performed and rate of hospitalization. For hospitalized children, we determined length of stay, mortality, and intensive care unit (ICU) transfer, as a marker of deterioration. We conducted bivariable analyses to identify risk factors for admission.
Results:
There were 201,551 ED visits among 129,938 children with complex CVD. Forty-eight percent of visits were for children < 5 years old. Thirty-seven percent of visits were for children with structural heart disease and 28% were for those with dysrhythmia. The mean number of encounters for children with complex CVD at each hospital varied (range 111 to 2,330 visits per year), as did the distribution of types of cardiac disease (e.g., range 16-42% and 11-47% for structural malformations and dysrhythmias, respectively). Most ED encounters had a primary diagnosis of a circulatory or respiratory illness (Figure 1). Resource utilization in the ED was high among all categories of CVD, with chest x-ray and complete blood count obtained in 46.7% and 54.6%, respectively. The overall rate of admission among the cohort was 58.8%, with 28.4% admitted to the ICU. Length of stay was > 7 days for 26.1% (Table 1). Younger age, white race, having an associated non-cardiac complex chronic condition and having multiple CVD types were associated with increased likelihood of admission (all p< 0.05; Table 2). Of admissions, 4.4% resulted in an ICU transfer after the first day; the rate of ICU transfer was highest (10.4%) among those with three or more CVD types. (Table 1).
Conclusion(s):
Children with complex CVD often require hospitalization and ICU level of care. These data begin to help understand how patient-level and encounter-level characteristics may impact illness severity and deterioration in this high-risk population.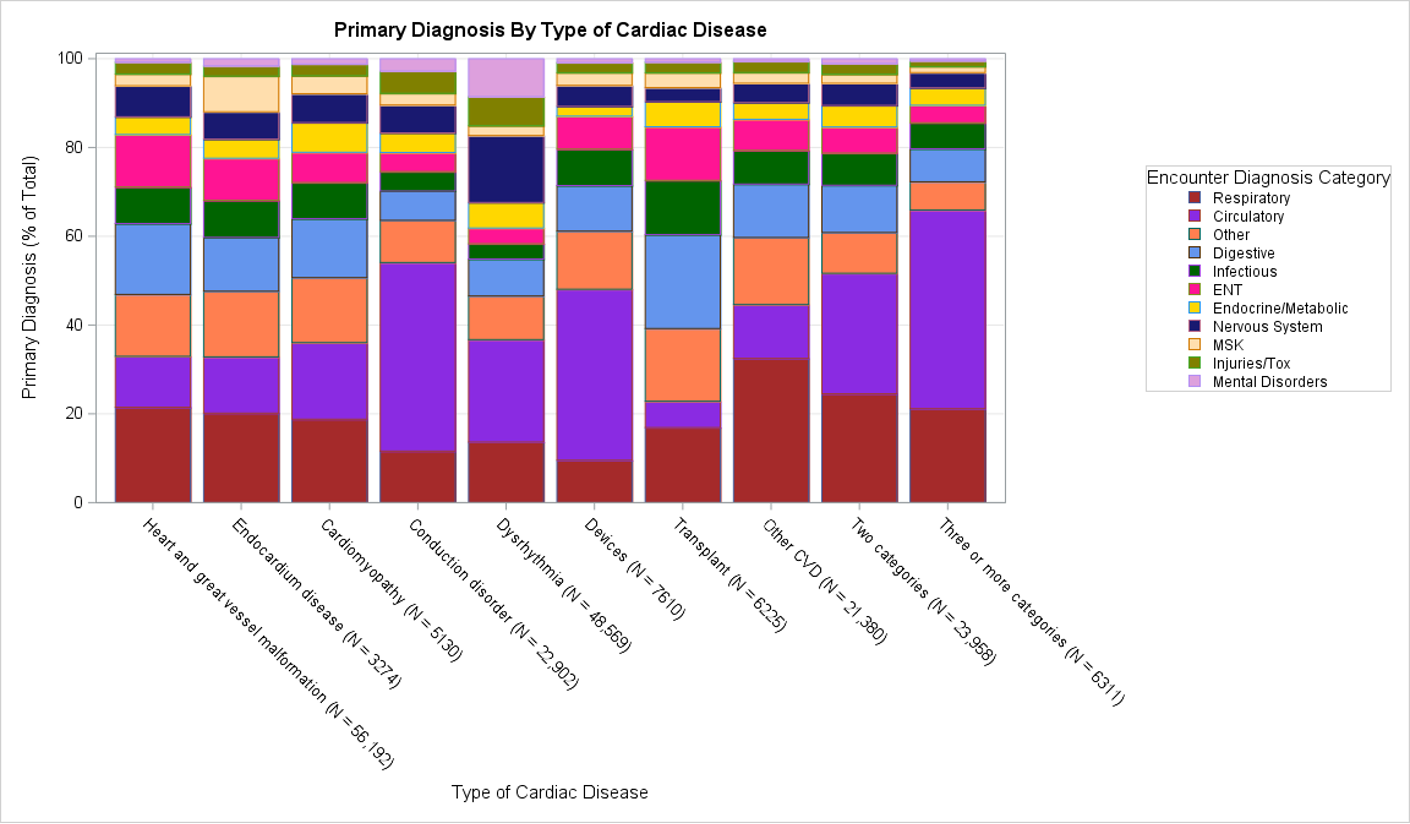
.png)
.jpg)
