Medical Education: Simulation & Technology
Medical Education 16: Potpourri 1
525 - Simulated Periviable Antenatal Co-Counseling for Families by Obstetric and Pediatric Trainees Using Standardized Patients
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 525
Publication Number: 525.424
Publication Number: 525.424
Julie Johnson Rolfes, University of Minnesota Masonic Children's Hospital, Minneapolis, MN, United States; Sabrina Burn, University of Minnesota, Minneapolis, MN, United States; Sarah N. Cross, Yale School of Medicine, Guilford, CT, United States
- JJ
Julie Johnson Rolfes, MD (she/her/hers)
Assistant Professor
University of Minnesota
Minneapolis, Minnesota, United States
Presenting Author(s)
Background: Obstetric and pediatric trainees have inconsistent and often infrequent opportunities to learn how to effectively partner antenatally with families facing a suspected periviable delivery, leading some trainees to graduate with an incomplete skillset. Simulation with live, standardized patients can offer a safe space to practice these high stakes, low frequency interactions, potentially improving trainees' skills.
Objective: To determine the feasibility, reception, and potential effectiveness of simulated, multidisciplinary, antenatal counseling for patients at high risk of periviable delivery.
Design/Methods: We designed a two-part, simulated patient encounter and invited trainees including senior Obstetrics and Gynecology (Ob-Gyn) residents, Maternal-Fetal Medicine (MFM) fellows and Neonatal-Perinatal Medicine (NPM) fellows to participate. Faculty from each of these programs were recruited to observe and provide feedback to trainees. On the day of simulation, trainees participated in an orientation and brief didactic, then were divided into multidisciplinary small groups who together counseled a simulated patient and her partner through a standardized, two-part, time-lapsed case of expected periviable delivery. Trainees completed pre- and post-simulation knowledge and comfort self-assessment surveys using a 5-point Likert scale. The post-simulation survey also assessed how well they received the experience. Evaluations were completed by faculty and simulated patients, as well.
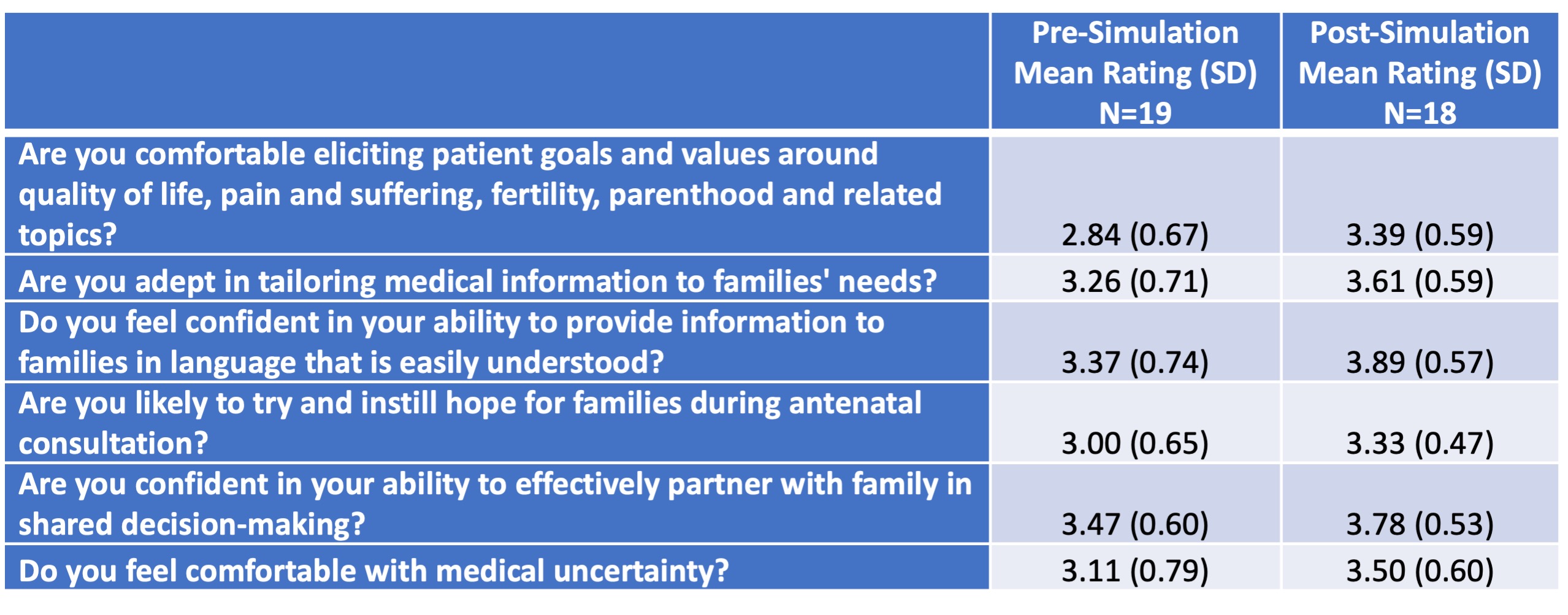
Results: A total of 19 trainees participated, including 11 Ob-Gyn residents, 2 MFM fellows and 6 NPM fellows. Eighteen participants completed both pre- and post-simulation surveys. Comparing the mean of Likert scale responses pre- and post-simulation, trainees reported improvement in their ability to: elicit patient goals and values around quality of life, parenthood, fertility and related topics; tailor their conversations to patient needs; use easily-understood language; instill hope; effectively partner with patients; and feel comfortable with medical uncertainty (Table 1). The post-simulation surveys reflected that trainees felt the experience provided a safe environment to practice counseling, and made them feel better prepared for counseling families in high-risk obstetrical scenarios during future clinical practice.
Conclusion(s): Providing obstetric and pediatric trainees with simulated periviable antenatal counseling experience is feasible, well received, and showed benefit across multiple factors that may improve trainees' ability to facilitate effective shared decision-making.