Neonatal Cardiac Physiology/Pathophysiology/Pulmonary Hypertension
Neonatal Cardiac Physiology/Pathophysiology/ Pulmonary Hypertension 5
121 - Indications and outcomes of neonatal ECMO for hypoxemic respiratory failure in California 2013-20
Publication Number: 121.427
- DS
Deepika Sankaran, MBBS MD DCH (she/her/hers)
Assistant Professor of Clinical Pediatrics
University of California, Davis, School of Medicine
University of California, Davis
Rocklin, California, United States
Presenting Author(s)
Background:
Extracorporeal membrane oxygenation (ECMO) is a life-saving intervention for critically ill neonates with hypoxemic respiratory failure (HRF) following failure of conventional medical management. Neonatal ECMO has been successfully used in reversible causes of HRF such as persistent pulmonary hypertension of the newborn (PPHN) secondary to meconium aspiration syndrome (MAS) and congenital diaphragmatic hernia (CDH).
Objective: To evaluate the incidence, trends, indications, risk factors, morbidities, and mortality after neonatal ECMO for HRF in California.
Design/Methods:
We collected data on maternal and infant characteristics, diagnoses and outcomes of neonates who underwent ECMO over an 8-year period (2013-2020) from the California Perinatal Quality Care Collaborative (CPQCC) database, a state-wide network of California’s neonatal intensive care units (NICUs). Descriptive statistics were performed using SAS 9.4, including analysis of associations between sociodemographic and clinical factors with ECMO use.
Results:
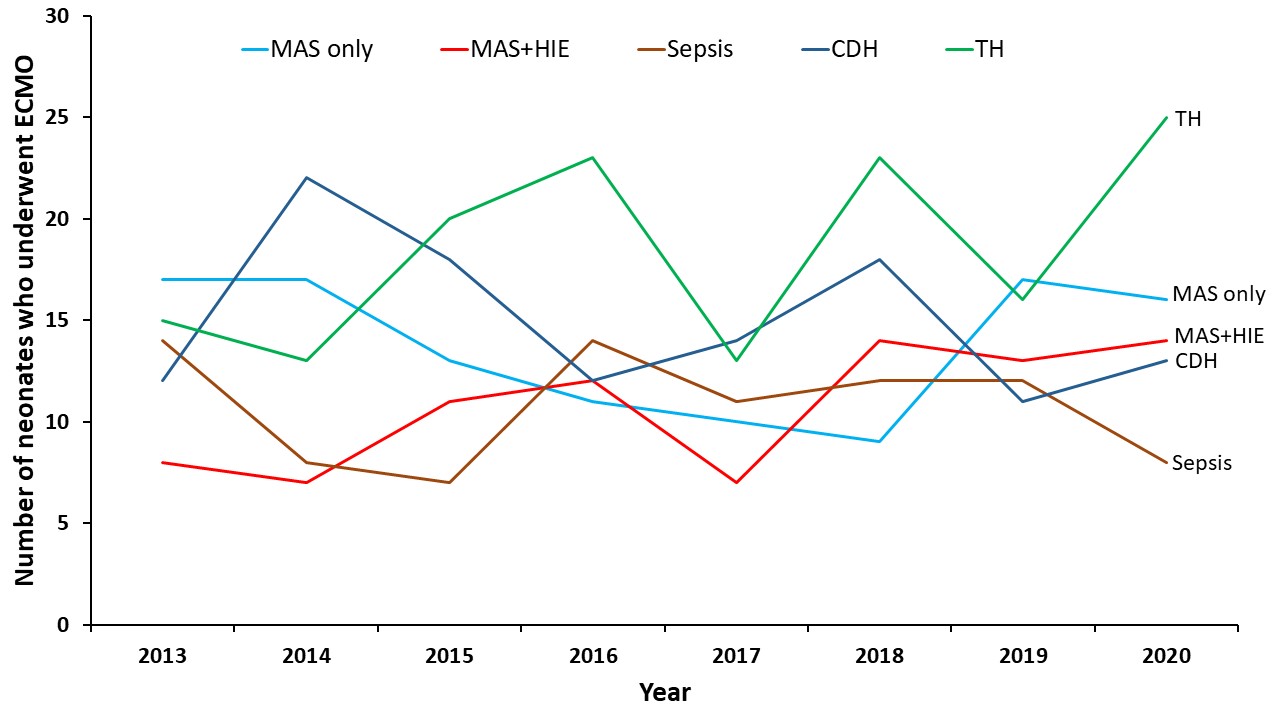
Maternal Black or Asian/Pacific Islander race was associated with higher incidence of inhaled nitric oxide (iNO) use and neonatal ECMO (table 1). Maternal hypertension and diabetes, fetal growth restriction and failure of progression of labor were associated with higher iNO use, whereas chorioamnionitis and fetal distress were associated with higher iNO use and neonatal ECMO. The leading indication for neonatal ECMO was therapeutic hypothermia (TH) following MAS and hypoxic ischemic encephalopathy (HIE) (148 cases), which was higher than CDH, (120 cases, figure 1). Mortality after ECMO was highest among neonates with CDH (21%, table 2) followed by MAS+HIE+TH (12.4%) compared to MAS without HIE (2.2%).
Conclusion(s): Therapeutic hypothermia is the leading association for HRF requiring neonatal ECMO in California, and the second leading cause of mortality following neonatal ECMO after CDH. TH causes pulmonary vasoconstriction and may exacerbate PPHN (Thoresen et al, Pediatrics 2000) potentially increasing the need for ECMO. Close hemodynamic assessments are warranted in neonates undergoing TH with HRF.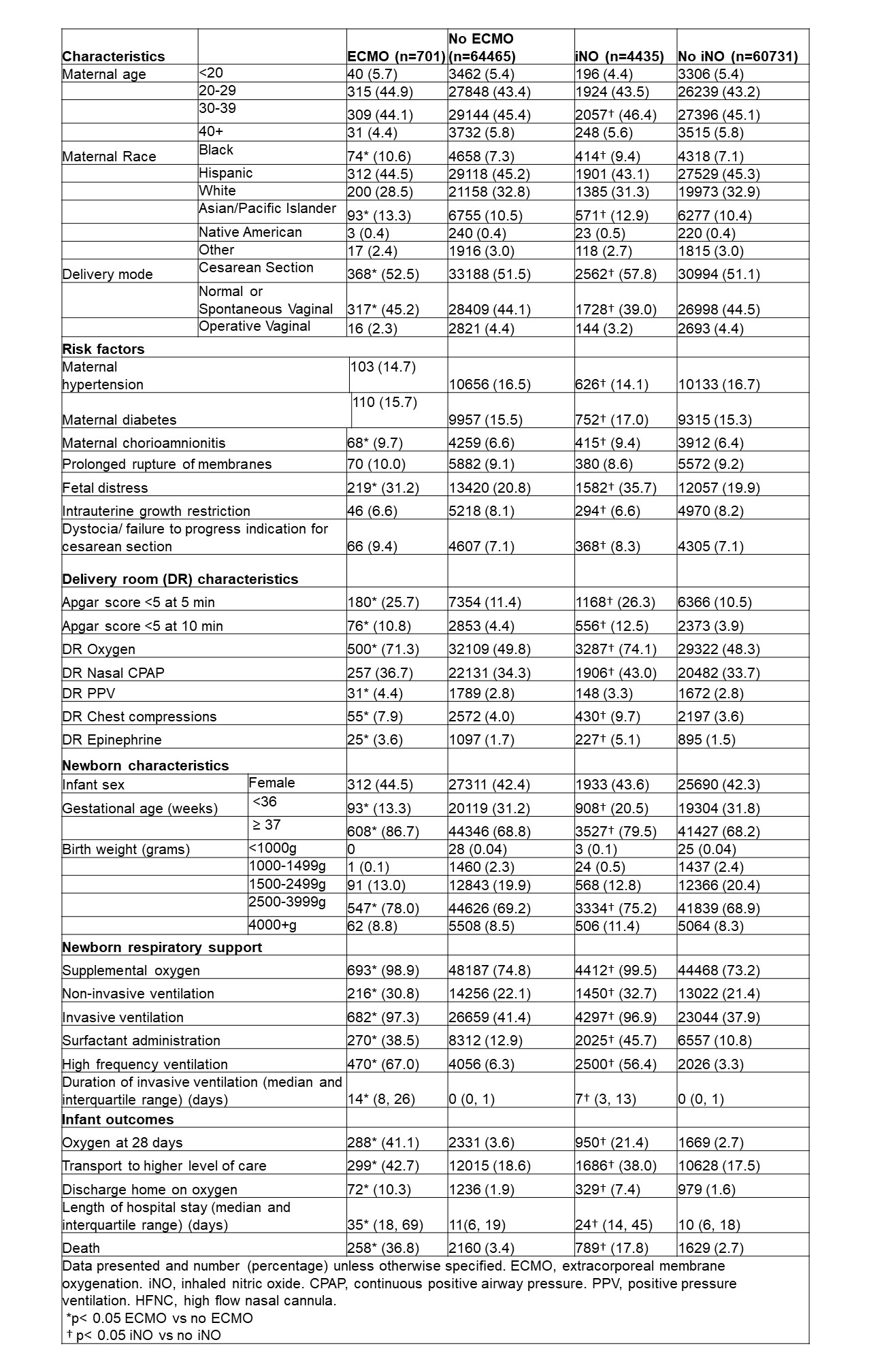
.jpg)
