Hospital Medicine: Clinical
Hospital Medicine 7
773 - Human Parechovirus Meningoencephalitis and Seizure Frequency during the 2022 outbreak – a Single-Center Retrospective Case Series
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 773
Publication Number: 773.416
Publication Number: 773.416
Nisha Shah, University of Kansas School of Medicine, Wichita, KS, United States; Nazeen S. Morelli, University of Kansas School of Medicine, Wichita, KS, United States; Jimmy Rong, University of Kansas School of Medicine, Wichita, KS, United States; Adam McClure, University of Kansas School of Medicine, Wichita, KS, United States; Julian Dedeaux, University of Kansas School of Medicine, Wichita, KS, United States; Sarah Krogman, University of Kansas School of Medicine, Wichita, KS, United States; Paul R. Teran, University of Kansas School of Medicine- Wichita, Wichita, KS, United States
.jpg)
Nisha Shah, MD (she/her/hers)
Resident
University of Kansas School of Medicine
Wichita, Kansas, United States
Presenting Author(s)
Background: Human Parechovirus (PeV) can affect neurologic, pulmonary, cardiac, and hepatic systems. Young infants are most vulnerable to PeV, but symptoms can be seen in children up to 2 years of age. Severe cases can progress to meningoencephalitis (ME), myocarditis, or hepatitis. In 2022, an outbreak of PeV ME occurred in young infants leading to hospitalization and complications.
Objective: To assess characteristics of pediatric PeV ME cases at Wesley Children’s Hospital (WCH) since introduction of the Biofire® FilmArray® Meningitis/Encephalitis Panel in April 2017 focusing on the 2022 outbreak.
Design/Methods: Retrospective chart review of cases of PeV ME at WCH from 2017 through 2022. Frequencies from 2022 cases were analyzed using t-test for continuous variables and Chi-squared tests for categorical variables.
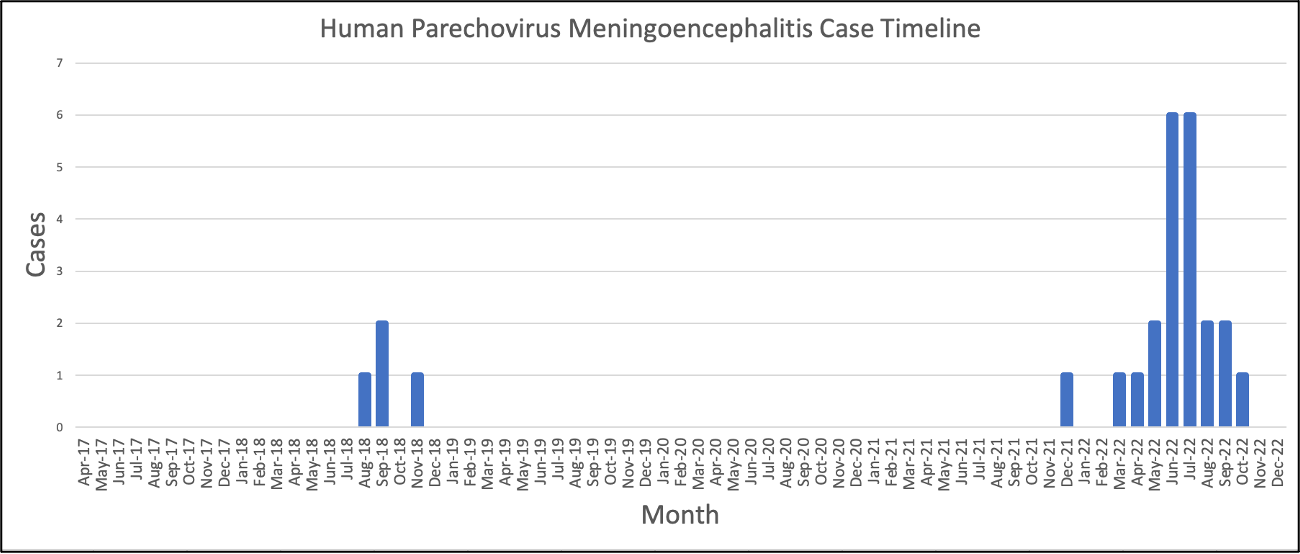
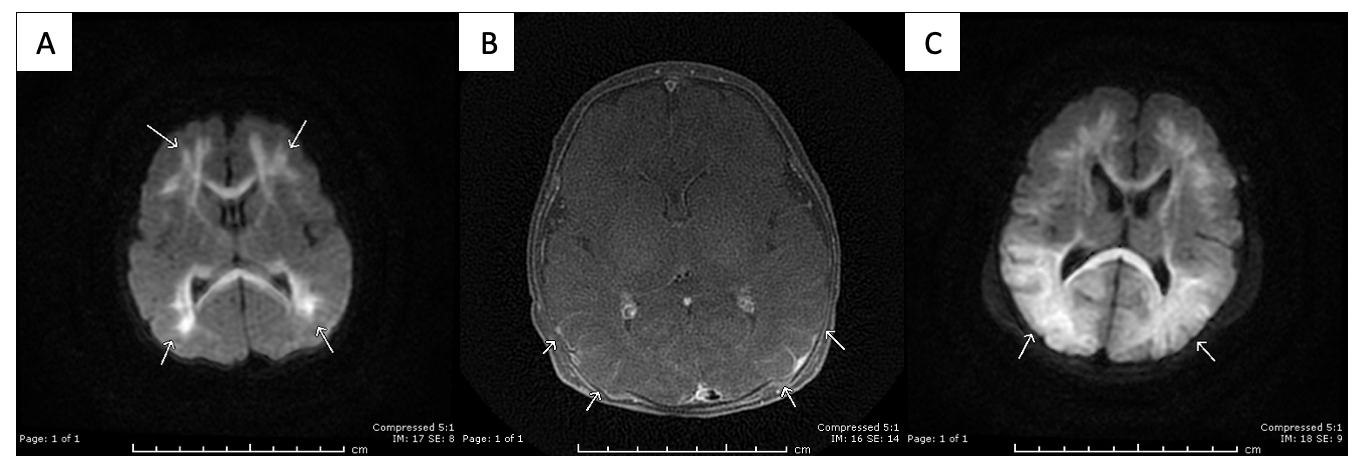
Results: In total, 26 cases of PeV ME were identified, 21 of which were in 2022 (Figure 1). No case prior to 2022 had seizures or severe outcomes. In 2022, eight patients had seizures, two of which also had hemodynamic instability requiring vasopressors, including one with confirmed myocarditis. One case of mild hepatitis was noted. All patients with seizures had brain magnetic resonance imaging (MRI) abnormalities consistent with PeV ME (Figure 2). Seven patients without seizures underwent MRI, of those two showed PeV ME abnormalities. Length of stay and intensive care utilization were increased in cases with seizures. Younger age and premature birth were associated with seizures. Patients with seizures were less likely to have fever and more likely to experience hypothermia (Table 1). There were no significant lab differences between the groups. Two cases showed neutrophilia, ten showed leukopenia, and 12 showed lymphopenia. No cases in 2022 involved a C-reactive protein greater than 20 mg/L or leukocytosis. No interpretable cerebrospinal fluid (CSF) white blood cell counts, protein, or glucose values were abnormal. In the seizure group, seven were discharged with antiepileptic medication and two required follow up with speech, physical, and occupational therapies for complications from PeV ME.
Conclusion(s): The 2022 PeV outbreak led to a wide range of outcomes with a high rate of seizures. Without reliable features of invasive infection, clinicians may rely on history, exam, and local epidemiology to guide diagnostic CSF testing to identify patients at risk of severe neurologic outcomes. Further research on the 2022 outbreak can help clinicians better understand PeV and risk factors for severe disease.
.png)
