Back
Background: Vaccine hesitancy is a significant barrier to COVID-19 vaccine uptake in the United States. Healthcare providers are the most trusted source of information, thus understanding provider’s comfort on COVID-19 vaccine counseling and developing an effective strategy is essential to increase vaccine uptake. The C-LEAR strategy (Counsel, Listen, Empathize, Answer, and Recommend) is an evidence-informed pneumonic developed for human papillomavirus vaccine counseling that we modified to improve COVID-19 vaccine counseling.
Objective: Evaluate the acceptability, intention to recommend the vaccine, and benefits of a one-hour in-person training to increase pediatric residents’ intent to and comfort with recommending the COVID-19 vaccine to parents for their children.
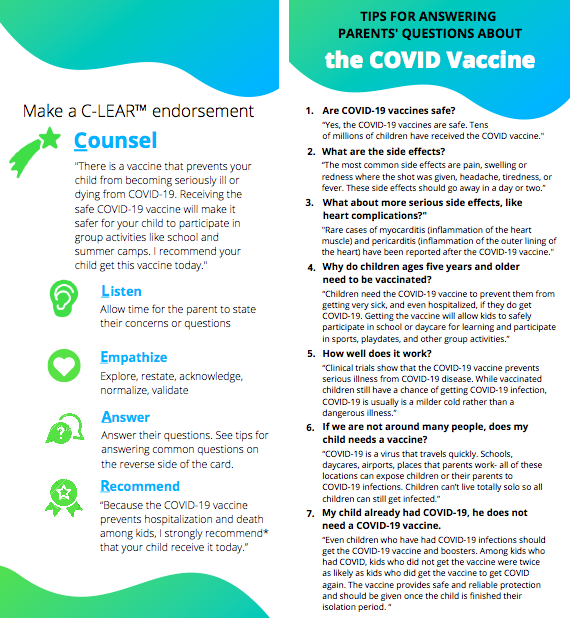
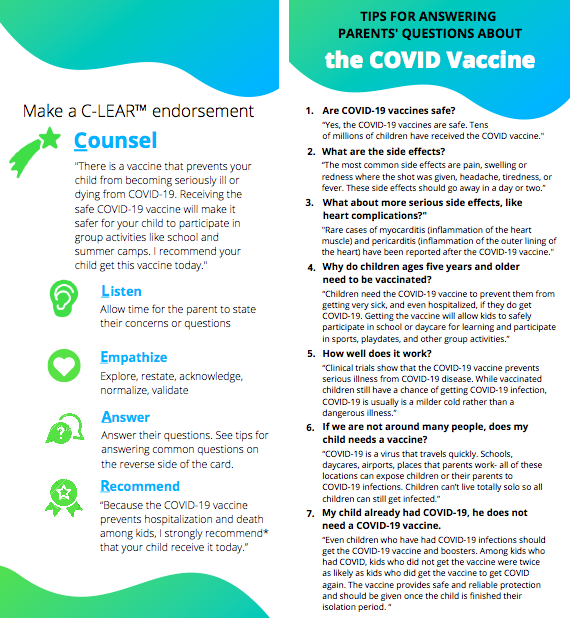
Design/Methods: We trained 26 pediatric residents to use the C-LEAR strategy for COVID-19 vaccine counseling. The training included a didactic session, demonstration of the C-LEAR strategy, and experiential role plays. Residents received a card summarizing the C-LEAR strategy with common questions and answers about the COVID-19 vaccine (Figure 1). Residents completed a survey before, immediately after, and 6 months after the training. A paired t-Test was used to compare the means between the pre-survey and immediate post-survey and the pre-survey and 6-month post-survey.
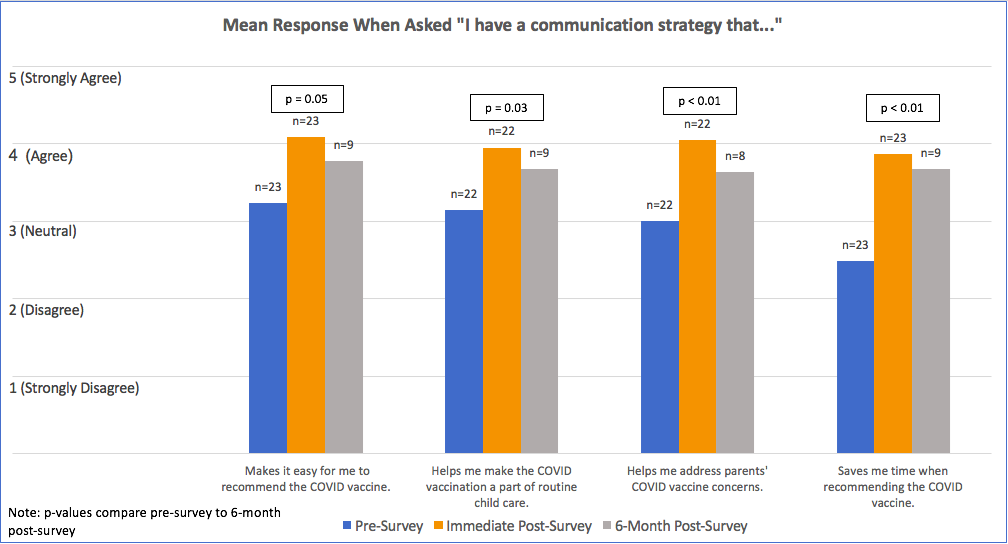
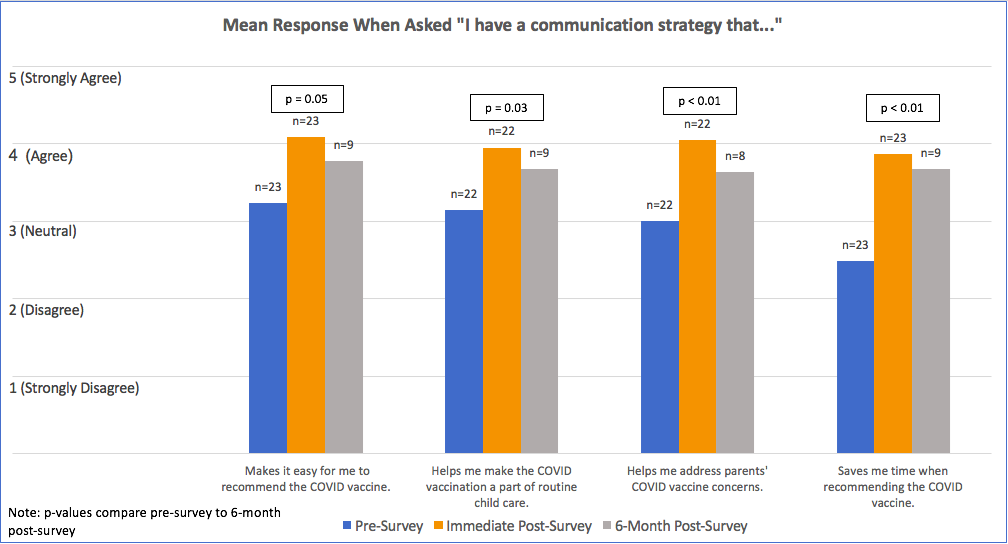
Results: Most residents had not received formal training in COVID-19 vaccine counseling (92%= 24/26) (Table 1). All of the residents completing the post-training survey agreed that the training was helpful and easy to understand (100%= 23/23). Immediately after, the majority agreed that the C-LEAR strategy would be more effective than their current practice in increasing COVID-19 vaccination (87% = 20/23) and intended to implement what they learned (100% = 23/23). More residents felt confident addressing parental concerns about COVID-19 vaccine 6 months after the training (78%= 7/9) than before training (23%= 6/26). There was a significant increase in the intent to recommend the vaccine 81-100% of the time in the next 30 days immediately after the training compared to before (p< 0.02), though significance was not seen 6 months after. There was a significant increase in various strategy benefits immediately after and 6 months after compared to before training including saving time (Figure 2).
Conclusion(s): Despite routine COVID-19 vaccine recommendations, most pediatric residents had not previously received formal education on vaccine counseling. Residents reported increased intent to recommend vaccination and improved counseling using the C-LEAR strategy.
.png)
Medical Education: Resident
Medical Education 13: Resident 4
474 - C-LEAR Communication: Improving COVID-19 Vaccine Counseling amongst Pediatric Residents
Monday, May 1, 2023
9:30 AM – 11:30 AM ET
Poster Number: 474
Publication Number: 474.421
Publication Number: 474.421
Alexandra K. Byrne, Nicklaus Children’s Hospital, Miami, FL, United States; Lindsay A. Thompson, Wake Forest Baptist Health - Brenner Children's Hospital, Winston Salem, NC, United States; Carma Bylund, University of Florida, Gainesville, FL, United States; Zachary Samuel. Schachter, University of Florida, Lutz, FL, United States; Marta D. Hansen, University of Florida College of Medicine, Gainesville, FL, United States; Stephanie A S. Staras, University of Florida College of Medicine, Gainesville, FL, United States

Alexandra K. Byrne, MD (she/her/hers)
Pediatric Hospital Medicine Fellow
Nicklaus Children’s Hospital
Miami, Florida, United States
Presenting Author(s)
Background: Vaccine hesitancy is a significant barrier to COVID-19 vaccine uptake in the United States. Healthcare providers are the most trusted source of information, thus understanding provider’s comfort on COVID-19 vaccine counseling and developing an effective strategy is essential to increase vaccine uptake. The C-LEAR strategy (Counsel, Listen, Empathize, Answer, and Recommend) is an evidence-informed pneumonic developed for human papillomavirus vaccine counseling that we modified to improve COVID-19 vaccine counseling.
Objective: Evaluate the acceptability, intention to recommend the vaccine, and benefits of a one-hour in-person training to increase pediatric residents’ intent to and comfort with recommending the COVID-19 vaccine to parents for their children.
Design/Methods: We trained 26 pediatric residents to use the C-LEAR strategy for COVID-19 vaccine counseling. The training included a didactic session, demonstration of the C-LEAR strategy, and experiential role plays. Residents received a card summarizing the C-LEAR strategy with common questions and answers about the COVID-19 vaccine (Figure 1). Residents completed a survey before, immediately after, and 6 months after the training. A paired t-Test was used to compare the means between the pre-survey and immediate post-survey and the pre-survey and 6-month post-survey.
Results: Most residents had not received formal training in COVID-19 vaccine counseling (92%= 24/26) (Table 1). All of the residents completing the post-training survey agreed that the training was helpful and easy to understand (100%= 23/23). Immediately after, the majority agreed that the C-LEAR strategy would be more effective than their current practice in increasing COVID-19 vaccination (87% = 20/23) and intended to implement what they learned (100% = 23/23). More residents felt confident addressing parental concerns about COVID-19 vaccine 6 months after the training (78%= 7/9) than before training (23%= 6/26). There was a significant increase in the intent to recommend the vaccine 81-100% of the time in the next 30 days immediately after the training compared to before (p< 0.02), though significance was not seen 6 months after. There was a significant increase in various strategy benefits immediately after and 6 months after compared to before training including saving time (Figure 2).
Conclusion(s): Despite routine COVID-19 vaccine recommendations, most pediatric residents had not previously received formal education on vaccine counseling. Residents reported increased intent to recommend vaccination and improved counseling using the C-LEAR strategy.
.png)