Hospital Medicine: Clinical
Hospital Medicine 5
750 - Validation of the Pediatric Hospital Admissions Survey of Experience (PHASE) Measure: An External Confirmatory Factor Analysis
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 750
Publication Number: 750.414
Publication Number: 750.414
Alaina M. Shine, Seattle Children's Hospital, University of Washington, Seattle, WA, United States; JoAnna Leyenaar, Dartmouth Health, Lebanon, NH, United States; Seneca D. Freyleue, Geisel School of Medicine at Dartmouth, South Burlington, VT, United States; Sonja I. Ziniel, University of Colorado School of Medicine - Department of Pediatrics, Aurora, CO, United States; Corrie E. McDaniel, University of Washington, Seattle, WA, United States

Alaina M. Shine, MD (she/her/hers)
Pediatric Hospital Medicine Fellow
Seattle Children's Hospital, University of Washington
Seattle, Washington, United States
Presenting Author(s)
Background: The home-to-hospital transition when a child needs hospitalization is a complex process for patients involving handoffs, changes in medical therapies, and stress to patients and families. The Pediatric Hospital Admission Survey of Experience (PHASE) measure is a 4-domain, 14-item quality measure that evaluates the quality of care delivered at the time of admission. While this quality measure has established validity evidence for admissions to general medical units, it has not yet been validated in other hospital settings.
Objective: To psychometrically validate the PHASE measure for patients admitted to an intensive care unit (ICU, neonatal or pediatric) or through interfacility transfer (IFT).
Design/Methods: We conducted a prospective study, July 2021-August 2022, using the Family Experience of Care Survey developed for the PHASE measure enrolling caregivers of eligible patients within 72 hours of hospital admission to a free-standing children’s hospital. Patients were eligible if admitted to an ICU (via the emergency department or IFT) or to the general medical or surgical ward through IFT. Confirmatory Factor Analysis (CFA) and indices of fit, including comparative fit index (CFI) and root mean squared error of approximation (RMSEA) were evaluated. Domain scores were calculated using a top-box approach, ranging from 0-1 with 1 representing 100% of respondents choosing the most-favorable answer.
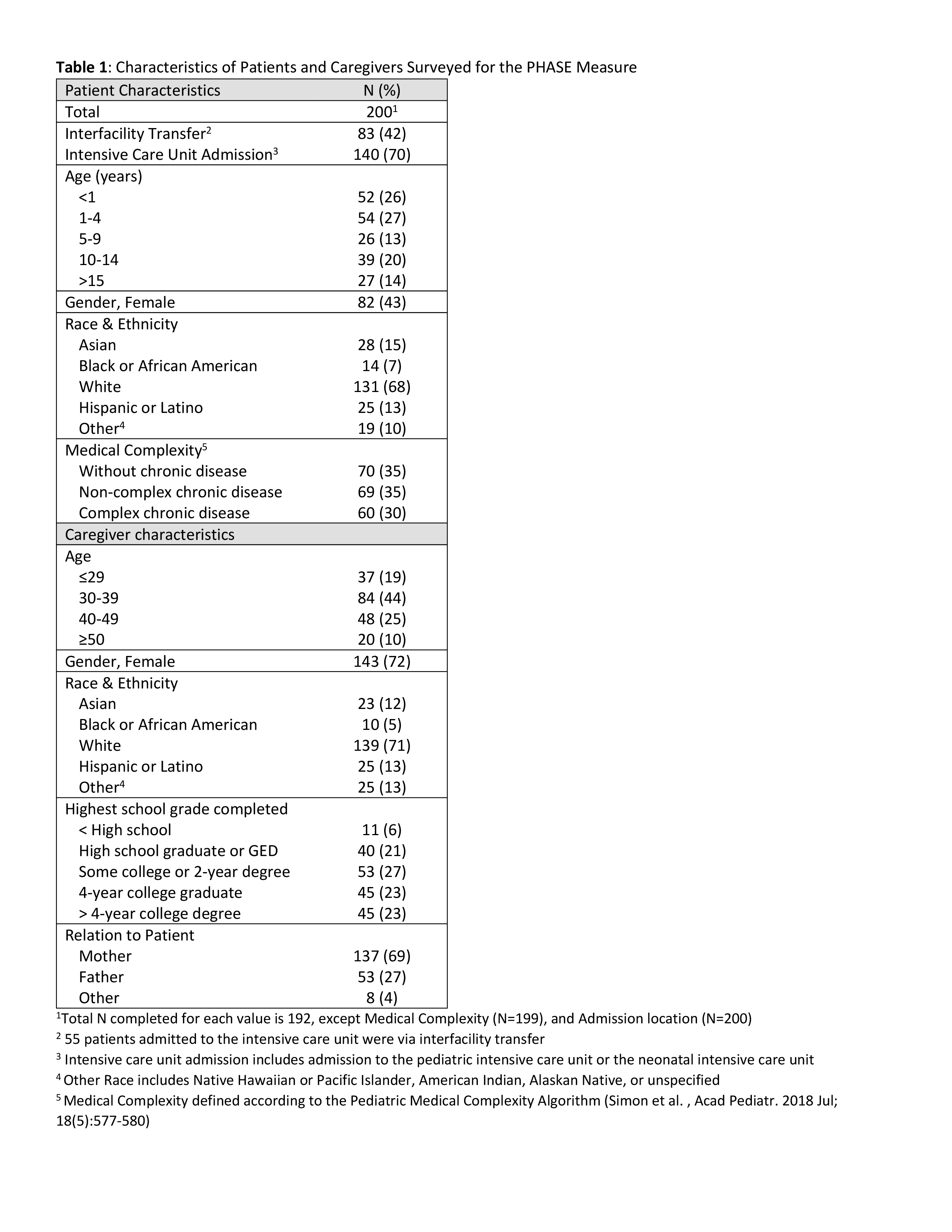
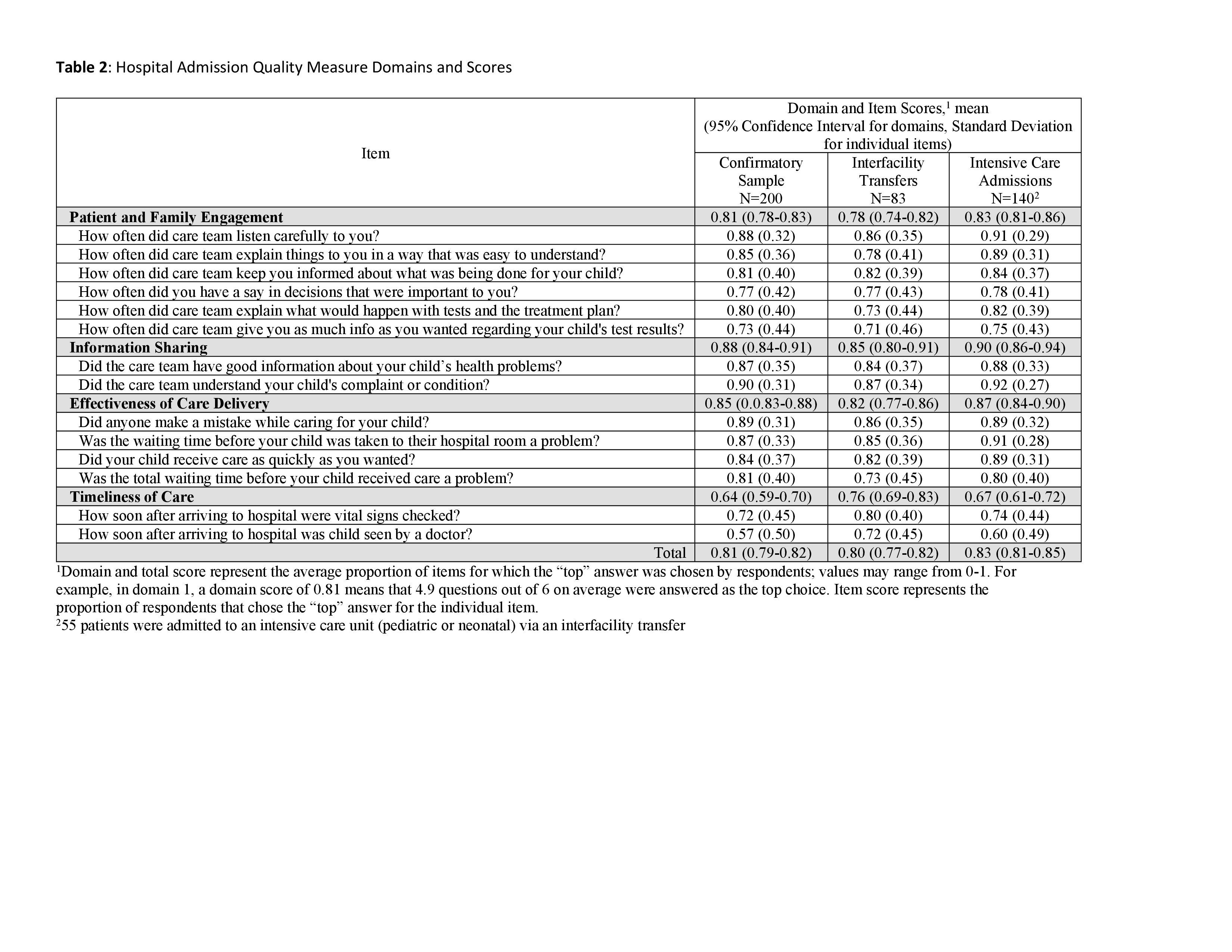
Results: Caregivers of 200 eligible patients completed the survey, 83 from caregivers after IFT and 140 within the ICU, including 55 patients admitted to the ICU via an IFT (Table 1). CFA resulted in confirmation of the 14-item measure within 4 domains: (1) Patient and Family Engagement, (2) Information Sharing, (3) Effectiveness of Care Delivery, and (4) Timeliness of care. Goodness of fit modeling demonstrated robust fit using the CFI (0.998) and RMSEA (0.053). Domain scores ranged from 0.64 (95% Confidence Interval (CI) 0.59-0.70) for Timeliness of Care to 0.88 (95% CI 0.84-0.91) in Information Sharing (Table 2).
Conclusion(s): The PHASE measure, a 4-domain caregiver-reported hospital admission quality measure, demonstrated validity in data collected within ICU settings and among patients admitted through interfacility transfer, building on previous validation work in general medical units. This measure can be used to evaluate the quality of transitions into the hospital and to focus admission quality improvement efforts