Neonatal Cardiac Physiology/Pathophysiology/Pulmonary Hypertension
Neonatal Cardiac Physiology/Pathophysiology/ Pulmonary Hypertension 3
85 - Association between time with open ductus arteriosus and congenital diaphragmatic hernia outcomes
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 85
Publication Number: 85.425
Publication Number: 85.425
Srirupa Hari Gopal, Baylor College of Medicine, Houston, TX, United States; Robert Tillman, Atrium Health Levine Children's Hospital, Charlotte, NC, United States; James D. Hammond, Baylor College of Medicine, Houston, TX, United States; Joseph Hagan, Baylor College of Medicine, Houston, TX, United States; Sharada H. Gowda, Baylor College of Medicine, Houston, TX, United States; NIdhy Varghese, Baylor College of Medicine, Houston, TX, United States; Caraciolo J.. Fernandes, Baylor College of Medicine, Houston, TX, United States

Srirupa Hari Gopal, MBBS
Fellow Physician
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background: Congenital diaphragmatic Hernia (CDH) is associated with pulmonary hypoplasia, leading to pulmonary hypertension (PH). While the presence of an open ductus arteriosus (DA) is helpful in the acute setting of CDH-PH to off load the failing right ventricle, the role of an open DA on long term outcomes in CDH has not been investigated.
Objective: Our objective was to examine associations of an open DA at 14 days and 30 days with long-term clinical outcomes in infants with in CDH.
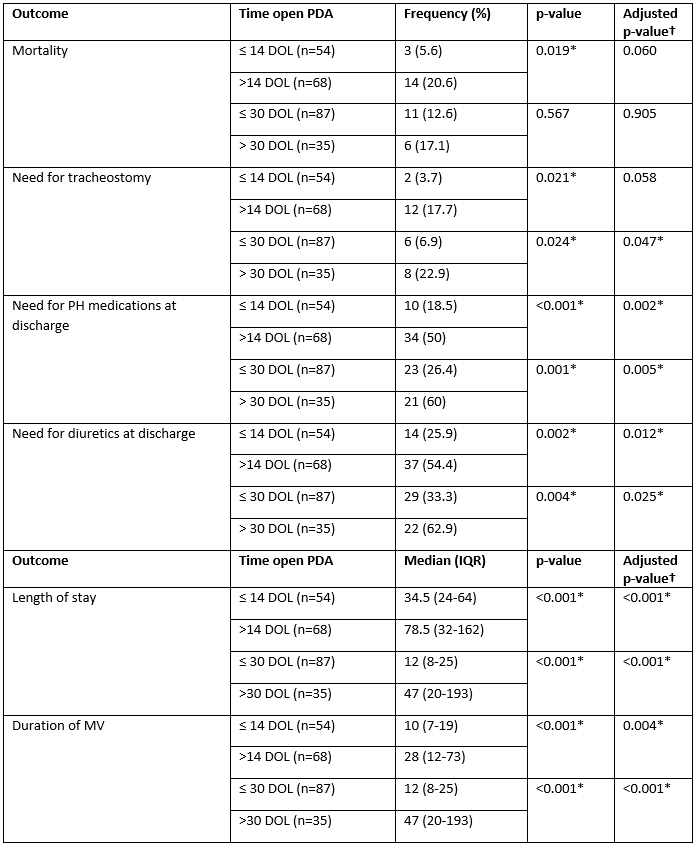
Design/Methods: This was a single center retrospective descriptive study of 122 patients with CDH (Table 1). Patients who received prostaglandins for patency of DA were excluded. Length of time with an open DA were dichotomized as ≤14 vs >14 days of life (DOL) and ≤30 vs >30 DOL. Fisher’s exact test and Wilcoxon rank sum test were used to compare the cohorts with categorical and quantitative variables, respectively. Logistic regression analysis was used to investigate the association of time with open DA with binary outcomes while correlation and linear regression analysis were used for continuous outcomes. Multiple linear regression and multiple logistic regression analysis were used to make these same comparisons for continuous and binary outcomes, respectively, after controlling for CDH severity.
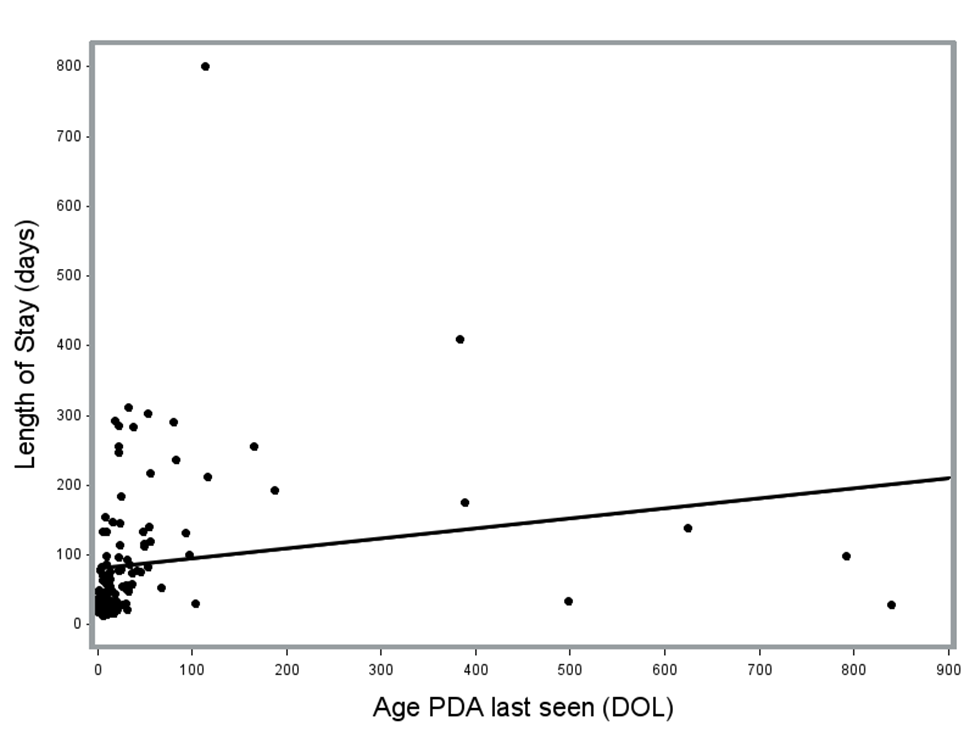
Results: In unadjusted comparisons to those with an open DA at ≤14 DOL, those >14 DOL had a higher risk of death, longer length of stay (LOS) and mechanical ventilation (MV) duration, and a greater need for tracheostomy, diuretics and PH medications at discharge. In comparison to patients with an open DA at ≤30 DOL, those >30 DOL had longer LOS, duration of MV, and greater need for tracheostomy, PH medications and diuretics at discharge. After controlling for CDH severity, patients with an open DA at >14 DOL had significantly longer LOS and duration of MV, greater need for PH medications and diuretics at discharge, and those with an open DA at >30 DOL had significantly longer LOS, duration of MV and greater need for tracheostomy, PH medications and diuretics at discharge (Table 2). For each additional day with an open DA, the predicted LOS increased by 0.15 days (p=0.04) (Figure 1).
Conclusion(s): Our study highlights the importance of identifying the role of an open DA in infants with CDH, given its association with important long-term outcomes. We speculate that an open DA can help in significant pulmonary hypertension, but on a long term can also contribute to lung injury. Either premise should prompt clinicians to investigate further to improve clinical outcomes in CDH.
.png)