Hospital Medicine: Hospital Medicine Quality Improvement
Hospital Medicine 7
779 - Understanding Provider Perspectives on Decreasing Overnight Vital Signs
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 779
Publication Number: 779.416
Publication Number: 779.416
Phuong Tran, Children's Hospital Colorado, Denver, CO, United States; Kelly R. S.. Wigglesworth, Children’s Hospital Colorado, Greenwood Village, CO, United States; A. Isabella Shanker, University of Colorado School of Medicine, Denver, CO, United States; Lauren Maloney, Children's Hospital Colorado, Denver, CO, United States; Lisa Greene, Children's Hospital Colorado, Aurora, CO, United States; Jillian M. Cotter, University of Colorado / Children's Hospital Colorado, Aurora, CO, United States; Kathleen G. Brimsek, University of Colorado School of Medicine, Aurora, CO, United States; Michael J. Tchou, University of Colorado Anschutz and Children's Hospital of Colorado, Aurora, CO, United States; Isabel Genecin, Children’s Hospital Colorado, Denver, CO, United States

Phuong Tran, MD (she/her/hers)
Resident
Children's Hospital Colorado
Denver, Colorado, United States
Presenting Author(s)
Background: Vital sign (VS) assessments are a common cause of sleep disruption in hospitalized children, however, obtaining VS every 4 hours (Q4H) on every inpatient is not evidence-based. At our institution, most patients receive standard Q4H VS assessments, even overnight.
Objective: Review the current practice and perceptions across clinical roles in regards to obtaining overnight Q4H VS assessments at a single large academic quaternary care children’s hospital.
Design/Methods: A survey was distributed to residents, fellows, hospitalists, advanced practice providers (APP), nurses, clinical assistants (CA), and behavioral health specialists (BHS) who practiced on inpatient general medical wards. Respondents rated on a 5 point likert scale how disruptive overnight VS were to healing, perceived necessity of overnight VS, and comfort level with skipping overnight VS in certain diagnoses. Descriptive statistics were used to assess demographics, perception of overnight vitals, and desirability of individual overnight vitals based on diagnoses.
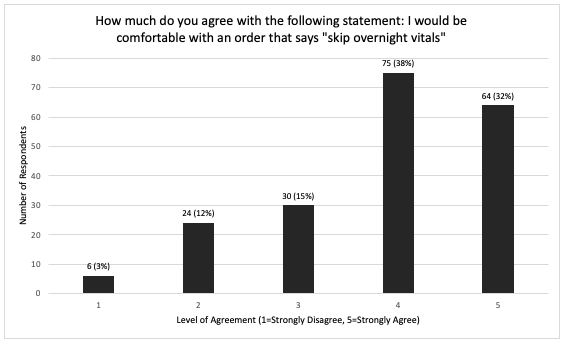
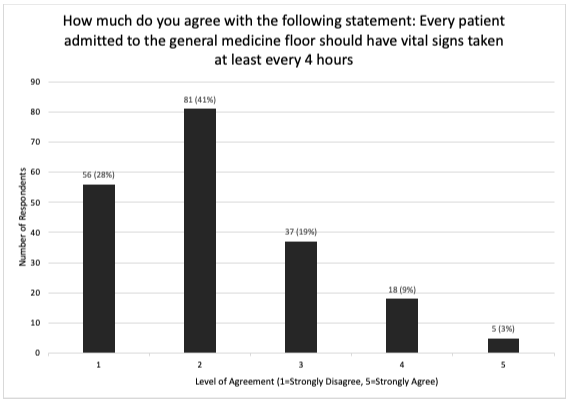
Results: A total of 200 respondents (41% nurses, 23% residents/fellows, 17% attendings, 11% CAs, 6% BHS, 1% APP, 1% nursing leadership) participated in the survey. The majority worked mostly night shifts or half nights (82%), and all had some exposure to night shifts. Across professions, 54% agreed (rated 4 or 5) that overnight vitals were disruptive to their patient’s healing, 69% disagreed (rated 1 or 2) that every patient should have VS taken at least Q4H (Figure 1), and 70% agreed they felt comfortable with an order to skip overnight vitals (Figure 2). Blood pressure was the most common VS respondents felt comfortable skipping. Respondents were most comfortable skipping overnight vitals for patients with constipation and least likely for patients with trauma (Figure 3). There was no significant difference in the responses by clinical role (p-values >0.05).
Conclusion(s): This study suggests that care providers feel comfortable decreasing overnight VS, especially for less acute disease processes. Thoughtful consideration to the utility of overnight VS assessments may help decrease disruption to patient sleep. Care providers should consider if VS should be further spaced >Q4H or skipped altogether for low acuity pathologies.
.png)