Back
Background: Pediatric patients have limited social agency and are uniquely vulnerable to health disparities. Previous work has shown associations between the childhood opportunity index (COI), a marker of neighborhood resources, and health outcomes.
Objective: We sought to identify associations between the COI, preventable hospitalizations, and excess healthcare cost.
Design/Methods: Retrospective cross-sectional study of the Pediatric Health Information Systems (PHIS) database including all inpatient hospitalizations among children < 18 years old between 1/1/2016 and 6/30/2022. Hospitalizations were grouped according to the 5 COI strata. Potentially preventable hospitalizations were identified based on ICD-10 codes in accordance with prior literature. Association between COI and preventable hospitalizations was assessed using multivariable logistic regression adjusting for age, sex, race, ethnicity, complex conditions, and insurance. Expected hospitalization proportions were normalized to the very high COI group, and excess hospitalizations, hospital days, deaths, and cost were determined.
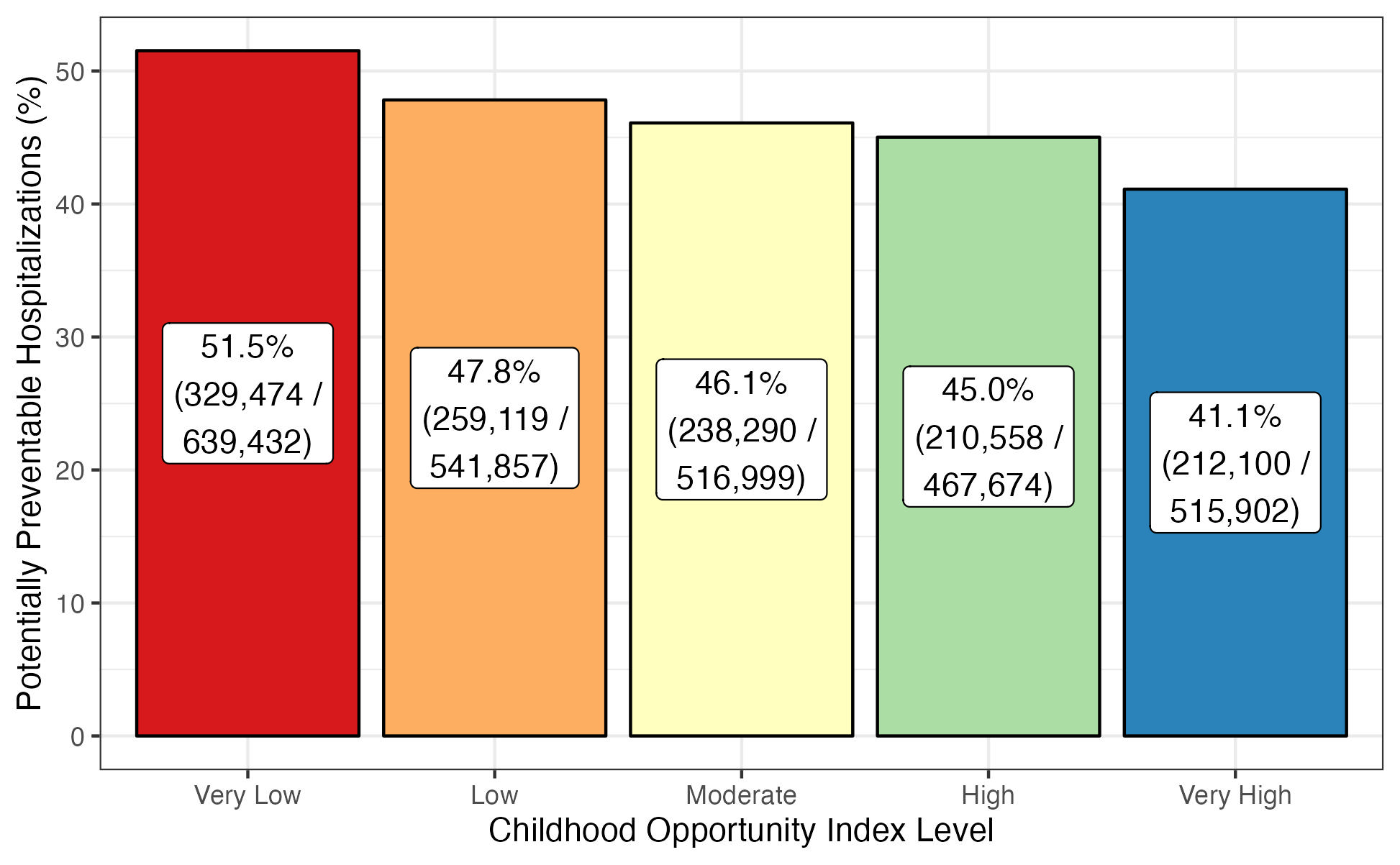
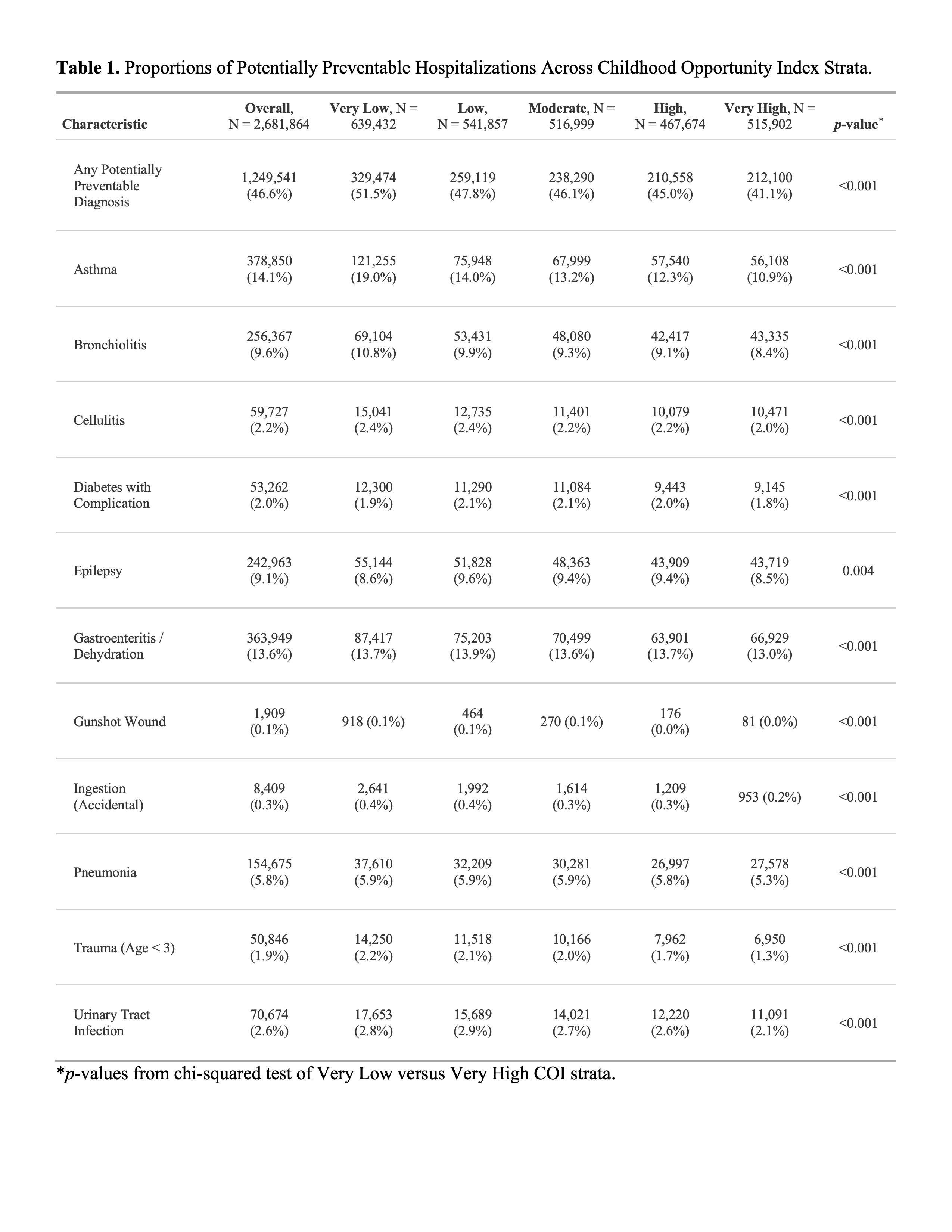
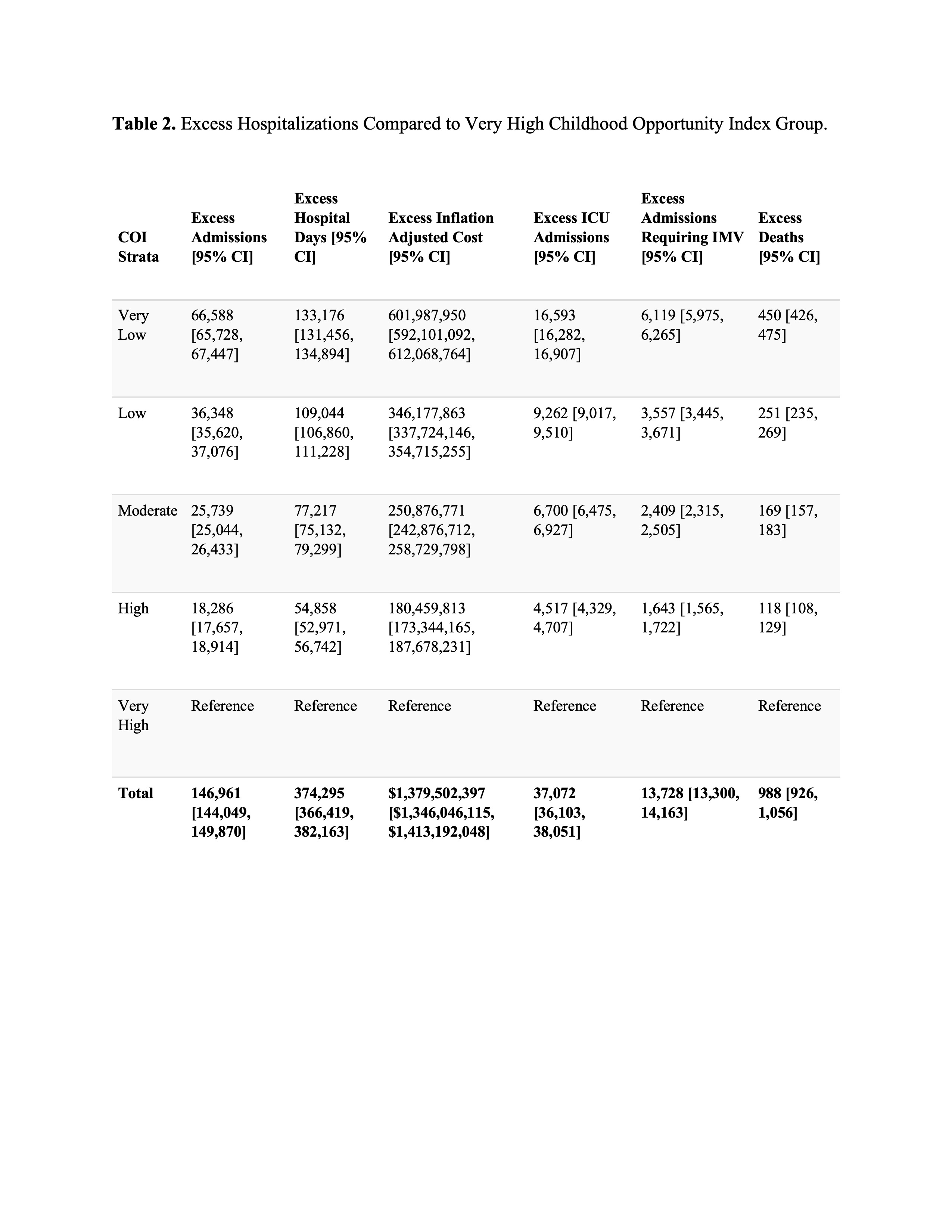
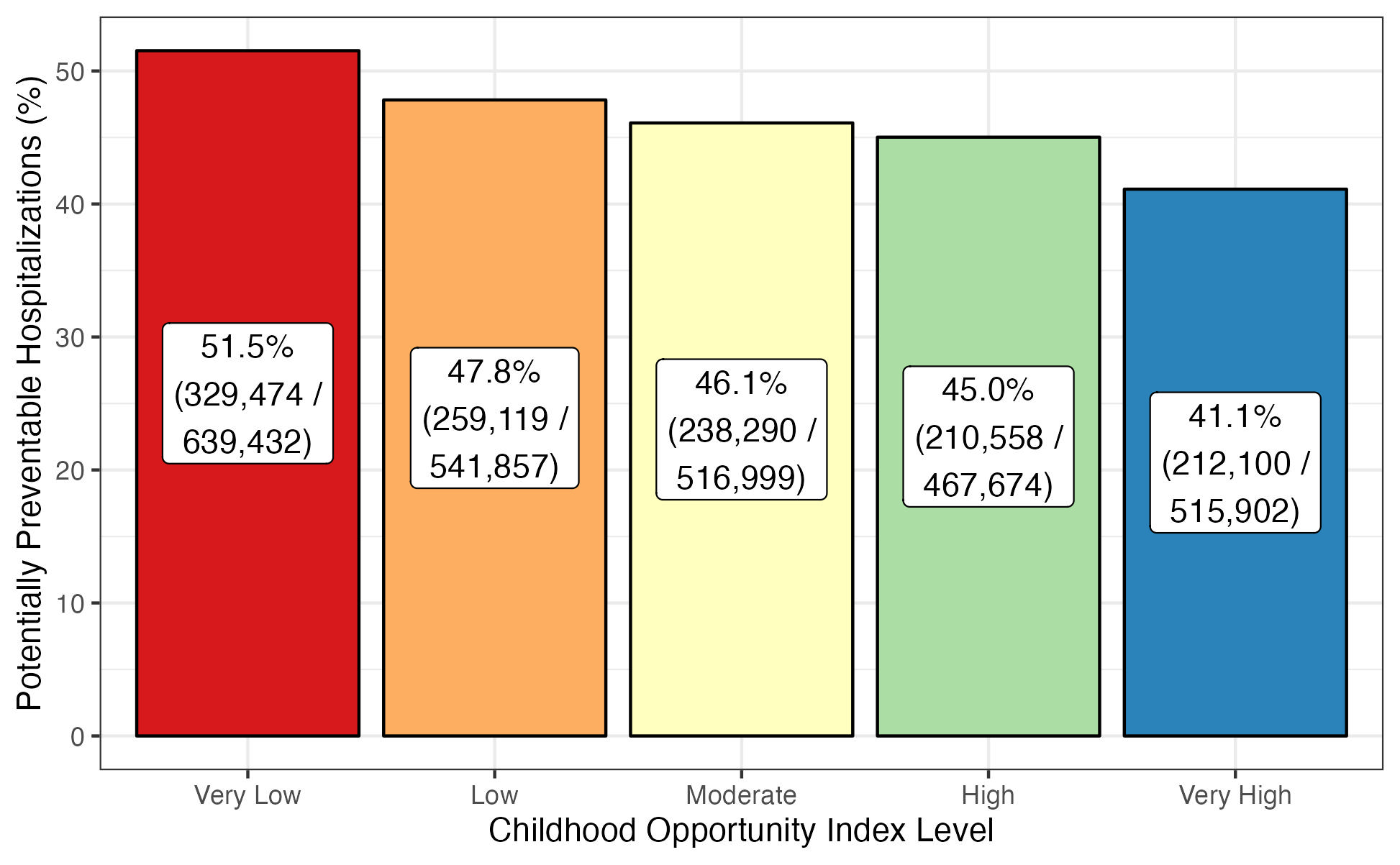
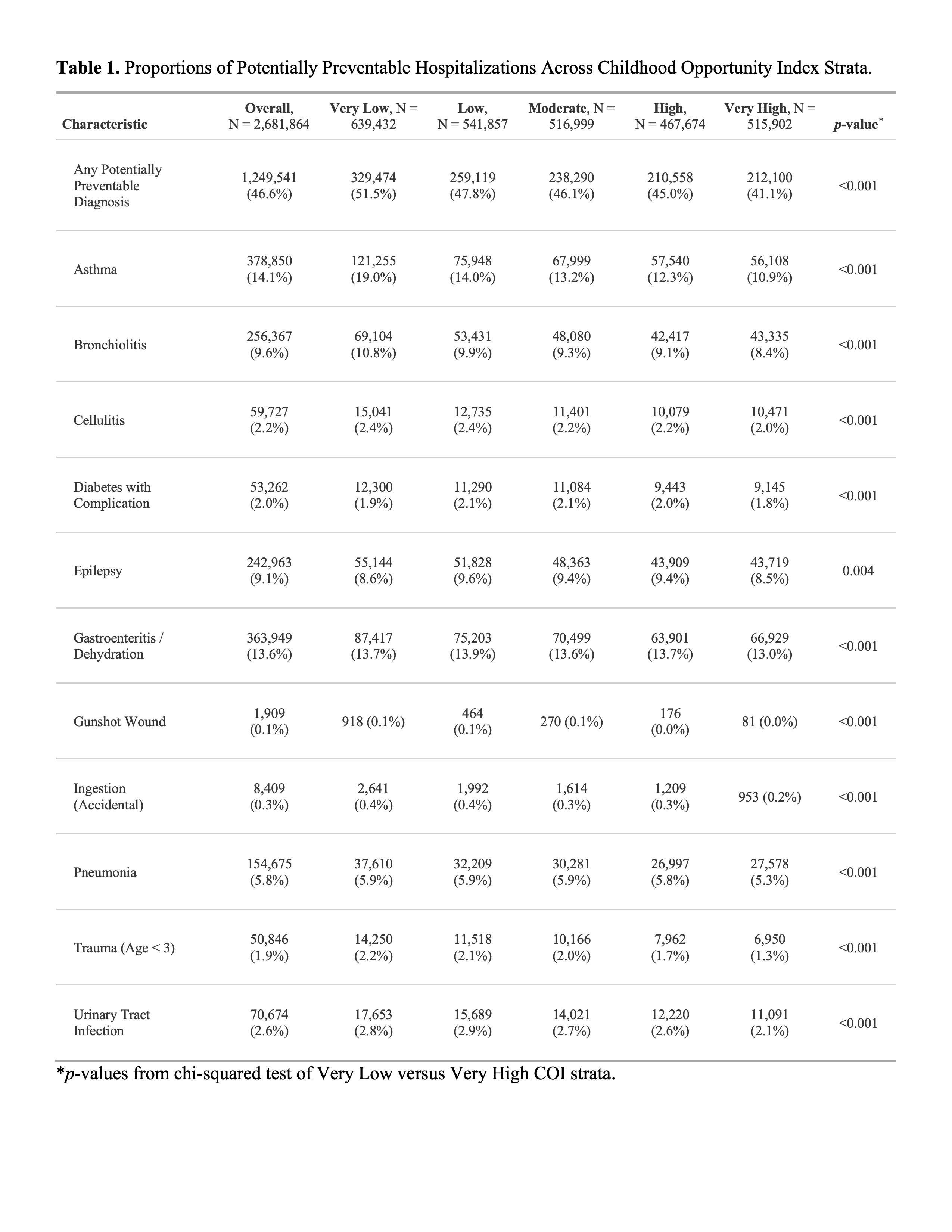
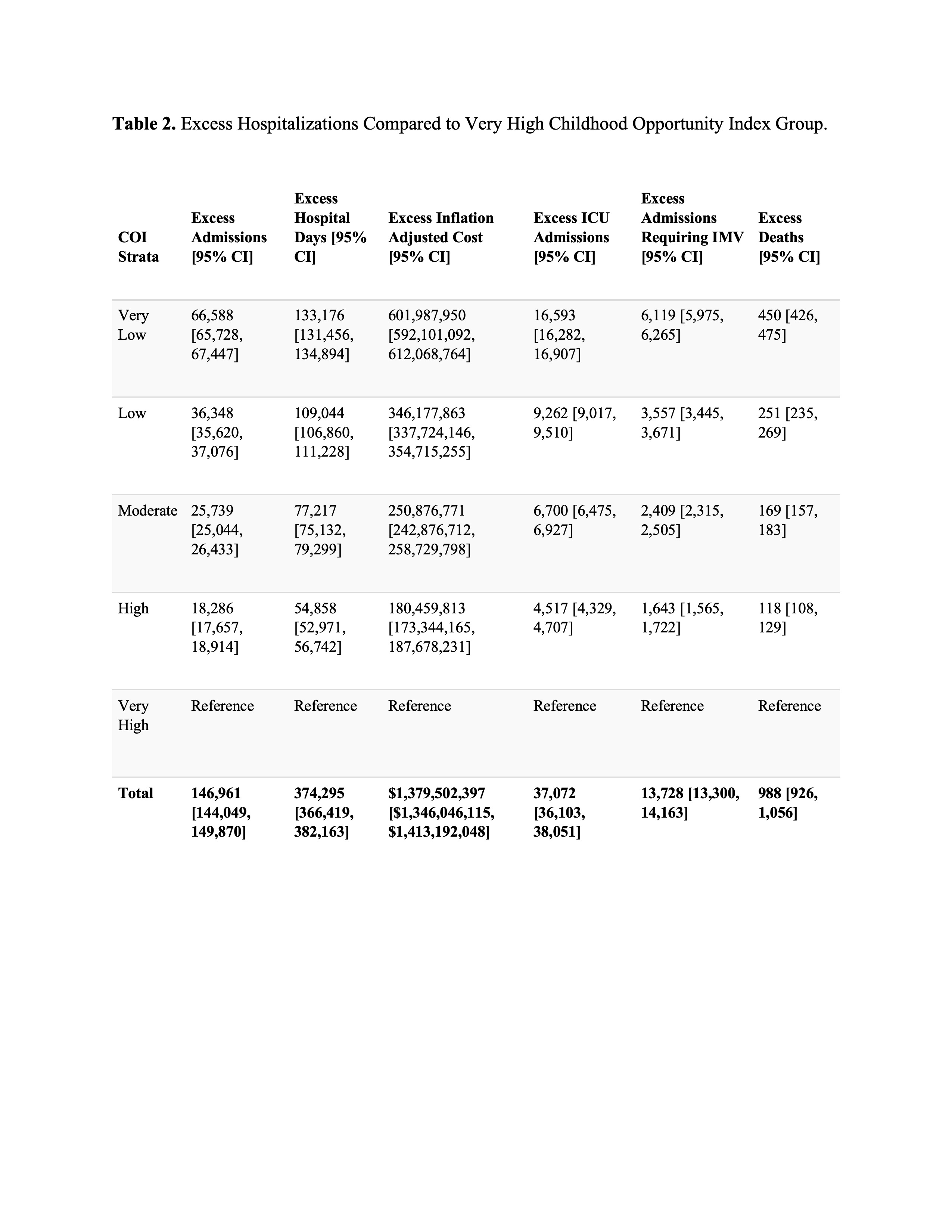
Results: Population data are reported as millions (M). There were 2.68M hospitalizations among 1.84M patients across 50 hospitals between 01/01/2016 and 6/30/2022. Of these, 46.6% (1.25M/2.68M) were potentially preventable according to ICD-10 diagnoses. Patients of Black race were overrepresented in lower COI strata, and patients of White and Asian American/Pacific Islander race were overrepresented in higher COI strata. Lower COI strata were associated with a higher proportion of potentially preventable hospitalizations, 51.5% (329,474/639,432) in the very low group compared to 41.1% (212,100/515,902) in the very high group (p < 0.001). After adjustment, lower COI strata were associated with higher odds of potentially preventable hospitalization, OR 1.221 [95% CI 1.210-1.231] in the very low COI group. Compared to the very high COI group, there were a total of 146,961 (95% CI 144,049-149,870) excess potentially preventable hospitalizations across all other COI strata, resulting in 374,295 (95% CI 366,419-382,163) excess hospital days, 988 (95% CI 926-1,056) excess deaths, and $1,379,502,397 (95% CI $1,346,046,115-$1,413,192,048) excess cost.
Conclusion(s): Children from lower COI strata were more likely to be hospitalized for preventable conditions. Targeted public health interventions to reduce these hospitalizations have the potential to reduce health inequities, and improve children's lives, with substantial cost avoidance.
Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 8
561 - Association Between Childhood Opportunity Index (COI) and Excess Pediatric Hospitalizations
Monday, May 1, 2023
9:30 AM – 11:30 AM ET
Poster Number: 561
Publication Number: 561.412
Publication Number: 561.412
Danielle Maholtz, Akron Children's Hospital, Akron, OH, United States; Christopher Page-Goertz, Akron Children's Hospital, Hudson, OH, United States; Michael L. Forbes, Akron Children's Hospital, Akron, OH, United States; Ryan Nofziger, Akron Children's Hospital, Akron, OH, United States; Michael T. Bigham, Northeast Ohio Medical University, Akron, OH, United States; Bryan P. McKee, Akron Children's Hospital, Akron, OH, United States; Sriram Ramgopal, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Jonathan H. Pelletier, Akron Children's Hospital, Akron, OH, United States

Danielle Maholtz, DO (she/her/hers)
Pediatric Critical Care Medicine Physician
Akron Children's Hospital
Akron, Ohio, United States
Presenting Author(s)
Background: Pediatric patients have limited social agency and are uniquely vulnerable to health disparities. Previous work has shown associations between the childhood opportunity index (COI), a marker of neighborhood resources, and health outcomes.
Objective: We sought to identify associations between the COI, preventable hospitalizations, and excess healthcare cost.
Design/Methods: Retrospective cross-sectional study of the Pediatric Health Information Systems (PHIS) database including all inpatient hospitalizations among children < 18 years old between 1/1/2016 and 6/30/2022. Hospitalizations were grouped according to the 5 COI strata. Potentially preventable hospitalizations were identified based on ICD-10 codes in accordance with prior literature. Association between COI and preventable hospitalizations was assessed using multivariable logistic regression adjusting for age, sex, race, ethnicity, complex conditions, and insurance. Expected hospitalization proportions were normalized to the very high COI group, and excess hospitalizations, hospital days, deaths, and cost were determined.
Results: Population data are reported as millions (M). There were 2.68M hospitalizations among 1.84M patients across 50 hospitals between 01/01/2016 and 6/30/2022. Of these, 46.6% (1.25M/2.68M) were potentially preventable according to ICD-10 diagnoses. Patients of Black race were overrepresented in lower COI strata, and patients of White and Asian American/Pacific Islander race were overrepresented in higher COI strata. Lower COI strata were associated with a higher proportion of potentially preventable hospitalizations, 51.5% (329,474/639,432) in the very low group compared to 41.1% (212,100/515,902) in the very high group (p < 0.001). After adjustment, lower COI strata were associated with higher odds of potentially preventable hospitalization, OR 1.221 [95% CI 1.210-1.231] in the very low COI group. Compared to the very high COI group, there were a total of 146,961 (95% CI 144,049-149,870) excess potentially preventable hospitalizations across all other COI strata, resulting in 374,295 (95% CI 366,419-382,163) excess hospital days, 988 (95% CI 926-1,056) excess deaths, and $1,379,502,397 (95% CI $1,346,046,115-$1,413,192,048) excess cost.
Conclusion(s): Children from lower COI strata were more likely to be hospitalized for preventable conditions. Targeted public health interventions to reduce these hospitalizations have the potential to reduce health inequities, and improve children's lives, with substantial cost avoidance.