Neonatal Cardiac Physiology/Pathophysiology/Pulmonary Hypertension
Neonatal Cardiac Physiology/Pathophysiology/ Pulmonary Hypertension 3
95 - Right ventricular dominance predicts postnatal intervention requirement in those with fetal suspicion of coarctation of the aorta
Publication Number: 95.425

Gabriel Altit, MDCM, MSc, FRCPC, FAAP (he/him/his)
Assistant Professor - Neonatologist - Montreal Children's Hospital
McGill University Faculty of Medicine and Health Sciences
Montreal, Quebec, Canada
Sam Amar (he/him/his)
Student
McGill University Faculty of Medicine and Health Sciences
Montreal, Quebec, Canada
Presenting Author(s)
Co-Author(s)
Background: The fetal diagnosis of coarctation of the aorta (CoA) is currently associated with a high false-positive rate.
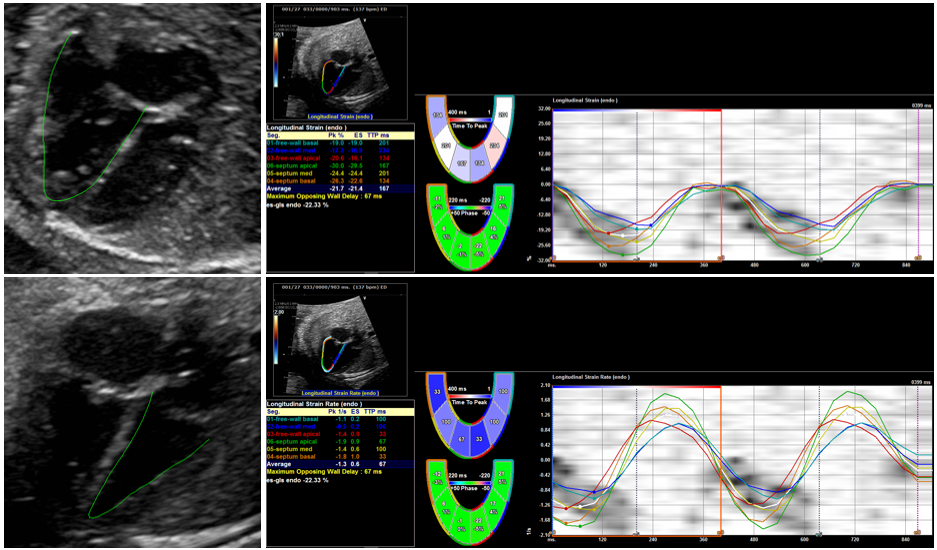
Objective: We sought to establish a set of traditional and speckle-tracking fetal echocardiography markers predictive of true CoA in neonates with a prenatal suspicion.
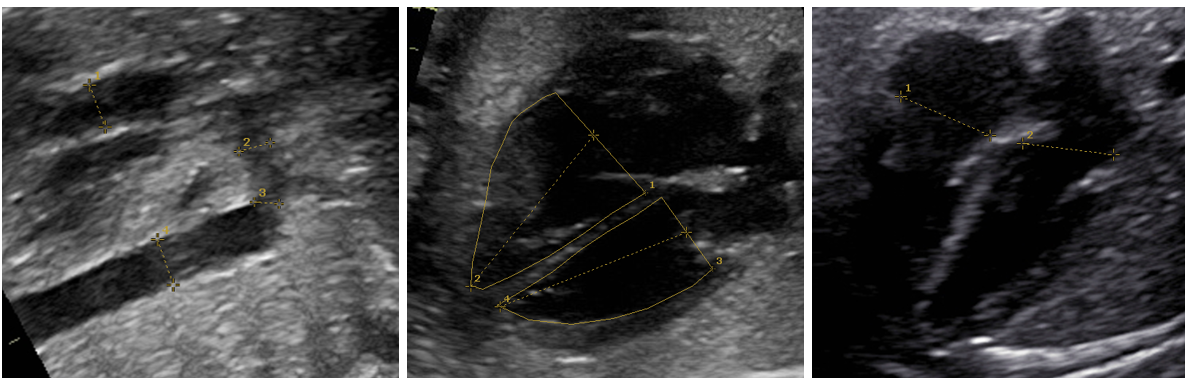
Design/Methods: Infants with a fetal echocardiography performed between October 2013 and May 2022 for an antenatal suspicion of CoA were included in this retrospective study. We compared the fetal ventricular and arch dimensions, as well as the deformation parameters using speckle-tracking echocardiography, of infants who required a postnatal intervention for their CoA to those who did not (control group). Data extractors were masked to the outcome. The first fetal echocardiogram available was used.
Results:
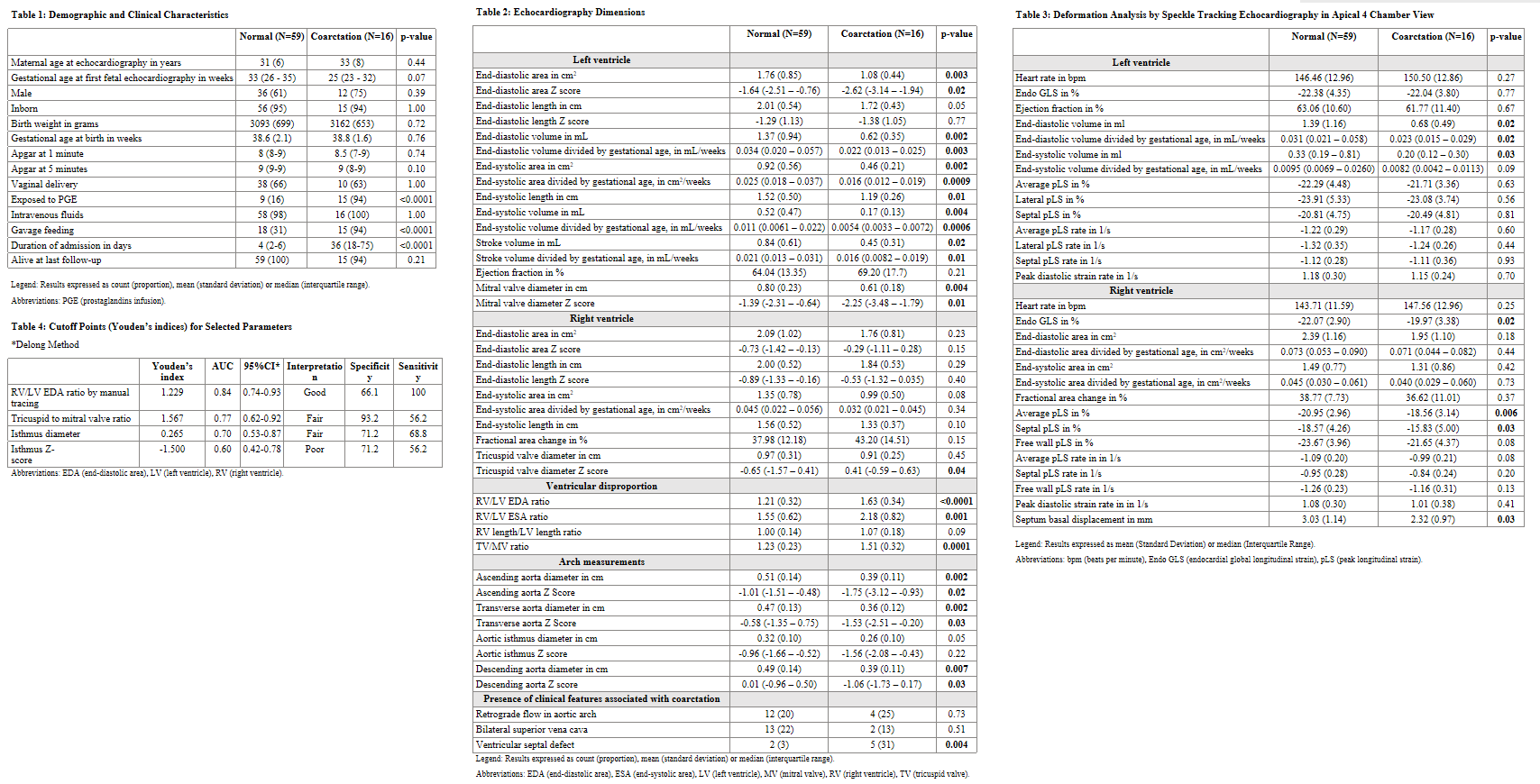
A total of 75 newborns were included, of which 59 (79%) had an aortic arch with non-significant obstruction upon ductal closure, and 16 (21%) underwent a neonatal intervention for a confirmed CoA. Compared to the controls, those with CoA had increased right to left ventricular dominance. Indeed, they had an increased right to left ventricular end-diastolic area [RV/LV EDA] ratio in the apical view (1.21 [0.32] vs 1.63 [0.34]; p< 0.0001) and an increased tricuspid to mitral valve diameter ratio (1.23 [0.23] vs 1.51 [0.32]; p=0.0001). The increased EDA ratio in those with CoA is due to these fetuses having a smaller left ventricle as opposed to a larger right ventricle. As such, the LV-EDA Z score was increased in the control group (-1.64 [-2.51 – -0.76] vs -2.62 [-3.14 – -1.94], p=0.02). A decreased right ventricular peak longitudinal strain was observed in the CoA group (-20.95 [2.96] vs -18.56 [3.14] %, p=0.006). No correlation was found between fetal isthmus diameter and the development of CoA. The RV/LV EDA ratio was the most sensitive predictor of CoA and identified all cases with CoA. Indeed, a cut-off >1.229 had a specificity of 66.1% and a sensitivity of 100% (receiver operating characteristic curve with an area under the curve of 0.84).
Conclusion(s): Right ventricular dominance, especially the right to left ventricular end-diastolic area ratio in the fetal apical 4-chamber view, is a useful tool to identify low-risk for a true CoA during fetal life.