Hospital Medicine: Clinical
Hospital Medicine 6
765 - Using Pediatric Early Warning Score to predict transfer to pediatric intensive care unit
Publication Number: 765.415

Jimin Lee, MD
Pediatric Hospital Medicine Fellow
The Children's Hospital at Montefiore
New York, New York, United States
Presenting Author(s)
Background:
Pediatric early warning score (PEWS) is a commonly used tool to identify children at risk of clinical deterioration on pediatric inpatient units. While PEWS is widely adopted, its performance characteristics vary in prior studies. To assess whether PEWS at the time of, or 2-4 hours prior to pediatric medical emergency team (PMET) activation predicted a pediatric intensive care unit (PICU) transfer or rapid escalation care.
Objective:
Design/Methods:
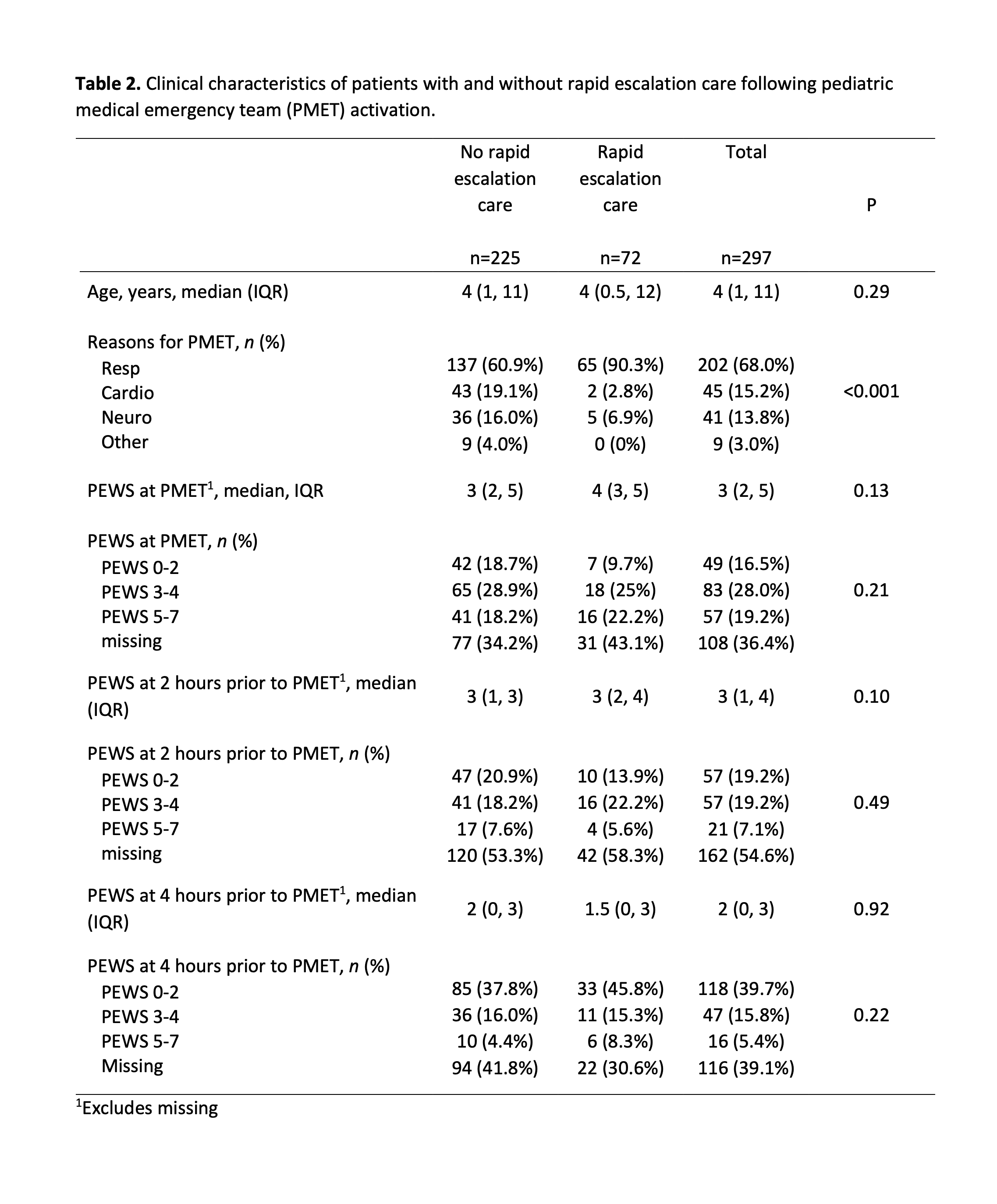
This retrospective cohort study was conducted at a metropolitan, quaternary care, academic children’s hospital where modified Brighton PEWS was implemented in 2016. Hospitalized patients ≤ 21 years old who had PMET activations between 8/1/2021 and 7/1/2022 were included. The primary outcome was PICU transfer. The secondary outcome was rapid escalation care (noninvasive ventilation, intubation, or vasopressor infusion) within 4 hours of PICU transfer. The variable of interest was the PEWS at the time of PMET activation, and 2 hours and 4 hours prior. Elevated PEWS was defined as PEWS ≥ 3, a locally determined threshold to increase frequency of assessment. PEWS ≥ 5 was also used as a cut off because it is a threshold to consider PMET activation. Chi-square, Fisher’s exact, and Mann-Whitney tests were used as appropriate to compare demographic and clinical characteristics between patients with and without the outcome. Sensitivity, specificity, and area under the receiver operating characteristic curve (AUROC) were calculated. 297 PMET activations took place in 244 unique patients. 185 (62.3%) PMET activations resulted in PICU transfer, and 72 (24.2%) received rapid escalation care. Respiratory illness was significantly more common in patients with PICU transfer (75.1% vs. 55.3%, p=0.001), and in patients who received rapid escalation (90.3% vs. 60.9%, p< 0.001) (Table 1). 81 (27.3%) PMET activations were in patients who did not have elevated PEWS within 4 hours prior to the activation. In patients with and without PICU transfer, there was no difference in PEWS distribution at the time of PMET, 2 hours and 4 hours prior (p >0.05) (Table 2). Similarly, there was no difference in the PEWS distribution in patients with and without rapid escalation care. The sensitivity and specificity of PEWS ≥ 3 and PEWS ≥ 5 within 4 hours prior to PMET for predicting PICU transfer or rapid escalation care was poor and the AUROC ranged 0.50–0.61 (Table 3). PEWS within 4 hours prior to PMET activation was a poor predictor of PICU transfer or rapid escalation care. Further work is needed to develop a more sensitive and specific tool.
Results:
Conclusion(s): 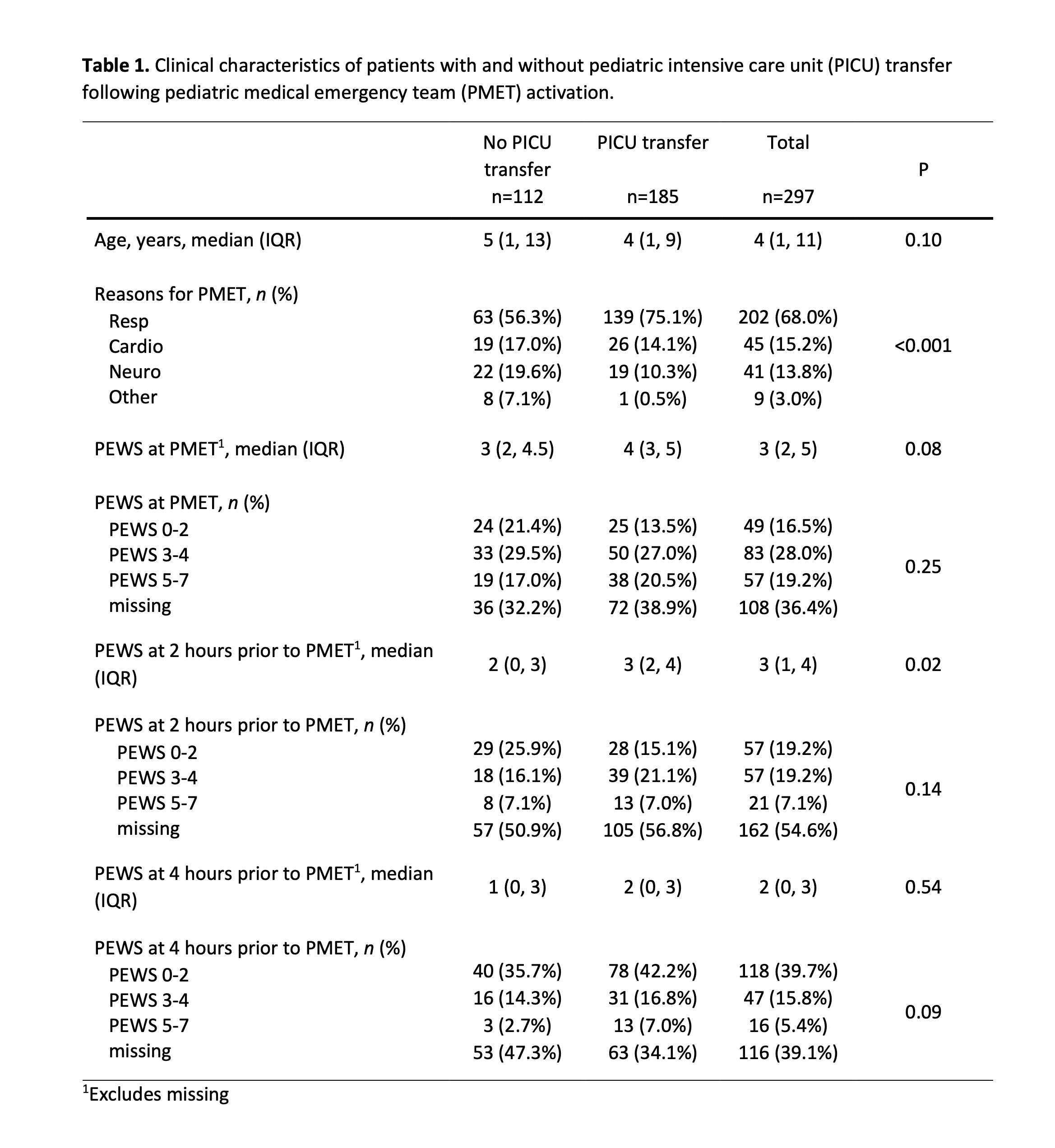
.png)
