Back
Background: Neonates with congenital diaphragmatic hernia (CDH) often have underlying pulmonary hypertension (PH) and cardiac dysfunction. Severity of PH and degree of ventricular dysfunction plays an important role in mortality and morbidity. These patients require varying levels of vasoactive medication support and are at high risk for adverse clinical outcomes. Need for multiple medications with high inotropic score (IS) and vasoactive inotropic score (VIS) has shown to have a predictive value in neonates undergoing congenital heart surgery and here we explore utilizing IS and VIS in patients with CDH.
Objective: Our objective was to investigate the utility of the inotropic score (IS) and vasoactive inotropic score (VIS) as tools to predict adverse clinical outcomes in CDH, and to correlate IS/VIS with postnatal echocardiographic variables.
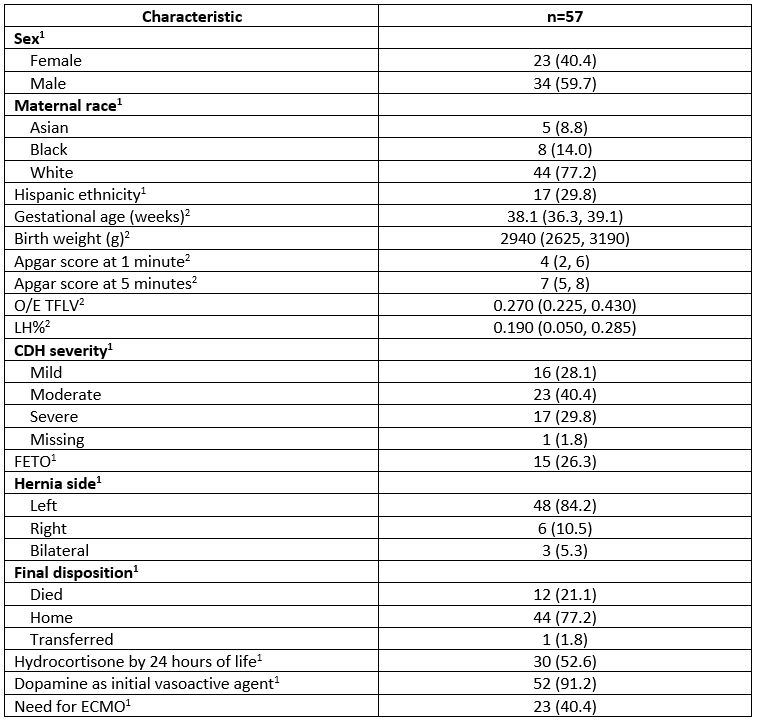
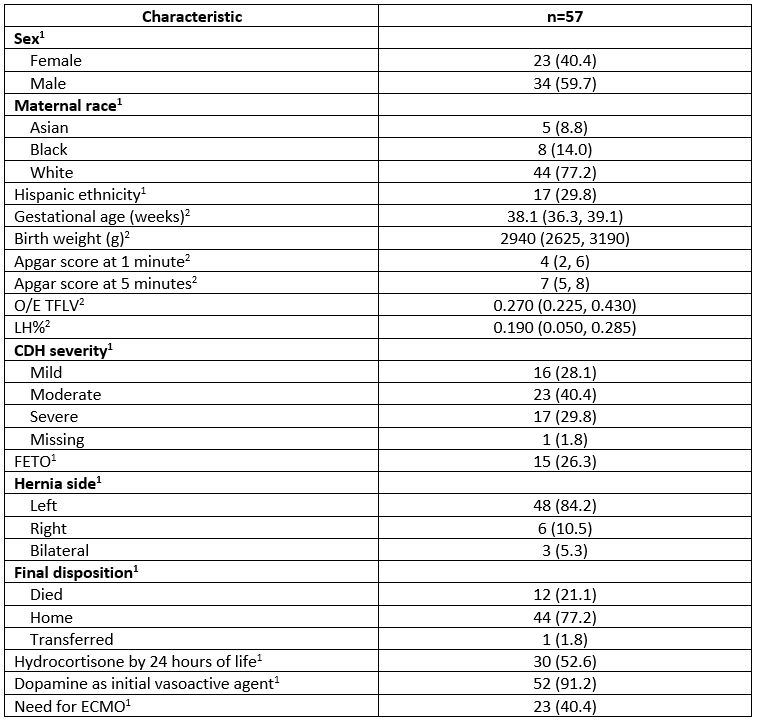
Design/Methods: This was a retrospective chart review of 57 patients (Table 1) with CDH. We calculated the IS/VIS at 6-, 12-, 24-, 48- hours of life (HOL), on the day of CDH repair and 24- and 48- hours after repair. The association of these scores with postnatal echocardiographic markers was analyzed using Pearson’s correlation and linear regression, while logistic regression was used for binary outcomes, and Cox proportional hazards regression was used to assess associations with survival.
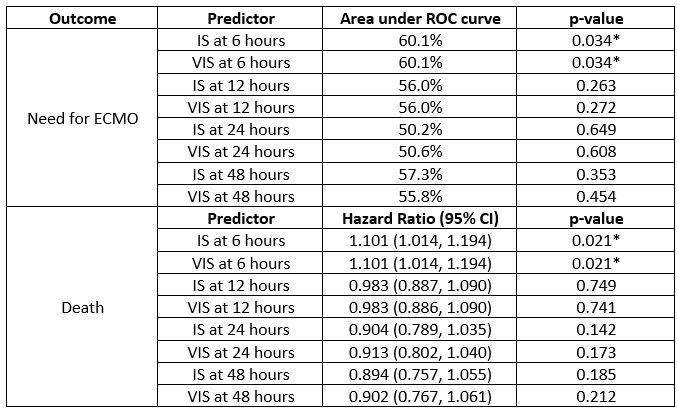
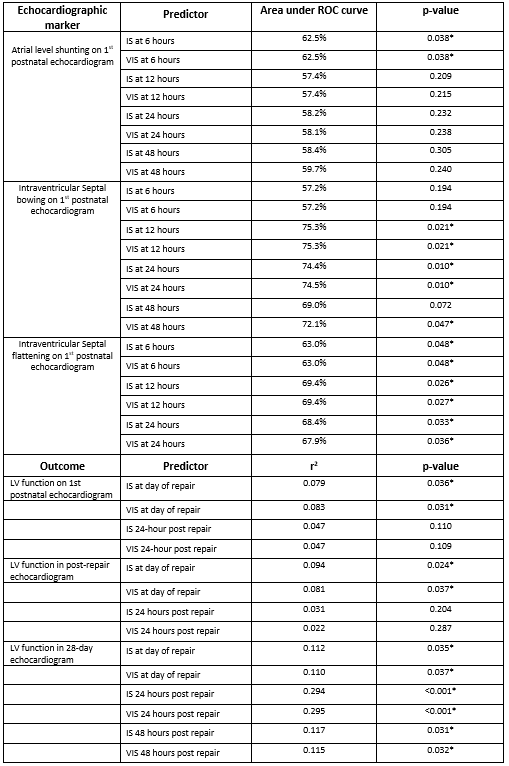
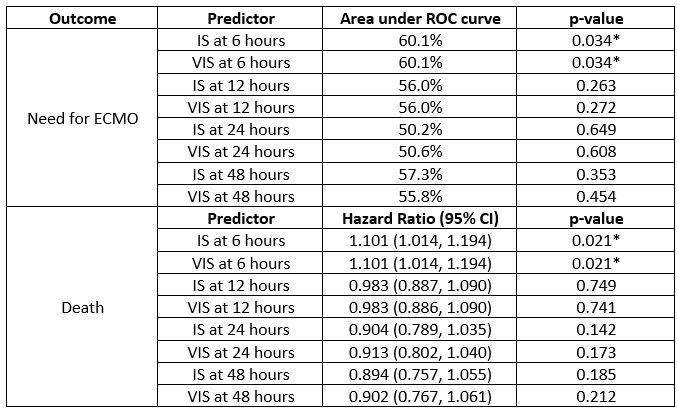
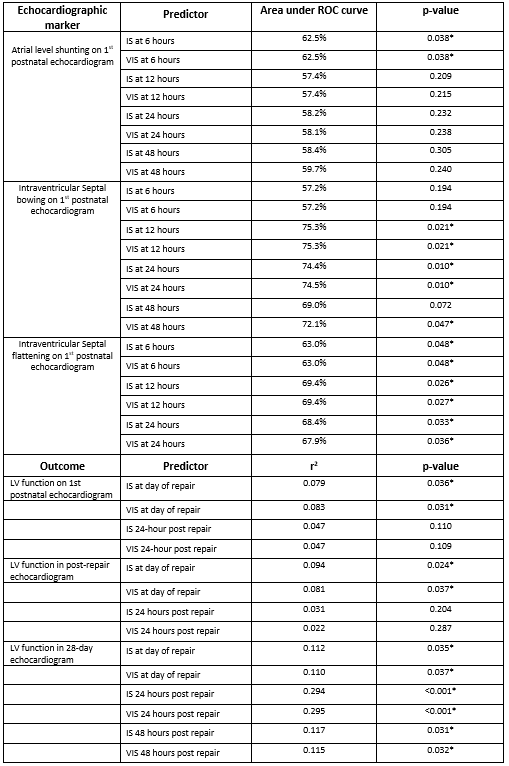
Results: Every one-unit increase in IS/VIS at 6 HOL was associated with a 13% increase in the odds of needing ECMO (p=0.034) and a 10.1% increase in risk of death (p=0.021) (Table 2). An increase in IS/VIS at 12-, 24- and 48- HOL was associated with posterior septal bowing in the first postnatal echocardiogram (p< 0.05 for all). We noted that left ventricle (LV) systolic function in the first postnatal echocardiogram was inversely related to IS (r= -0.281, p=0.036) and VIS (r= -0.288, p=0.031) calculated on the day of repair. Similarly, increase in IS (r= -0.307, p=0.024) and VIS (r= -0.285, p=0.037) on the day of repair was associated with decreased LV function on the post-repair echocardiogram (Table 3).
Conclusion(s): This study showed a significant association between IS/VIS obtained at various time points with clinical outcomes and echocardiographic findings in CDH, which can help guide prognosis and management in this patient population.
Neonatal Cardiac Physiology/Pathophysiology/Pulmonary Hypertension
Neonatal Cardiac Physiology/Pathophysiology/ Pulmonary Hypertension 3
92 - Inotropic Score and Vasoactive Inotropic Score as Predictors of Outcomes in Congenital Diaphragmatic Hernia: A Single Center Retrospective Study
Monday, May 1, 2023
9:30 AM – 11:30 AM ET
Poster Number: 92
Publication Number: 92.425
Publication Number: 92.425
Srirupa Hari Gopal, Baylor College of Medicine, Houston, TX, United States; Cynthia L. Toy, Texas Children's Hospital, Houston, TX, United States; Morcos Hanna, Texas Children's Hospital, Houston, TX, United States; Betul Yilmaz Furtun, Texas Children's Hospital, Houston, TX, United States; Joseph L. Hagan, Baylor College of Medicine, Houston, TX, United States; Ahmed A. Nassr, Baylor College of Medicine / Texas Children’s Hospital, Houston, TX, United States; Caraciolo J.. Fernandes, Baylor College of Medicine, Houston, TX, United States; Sundeep Keswani, Baylor College of Medicine, Houston, TX, United States; Sharada H. Gowda, Baylor College of Medicine, Houston, TX, United States

Srirupa Hari Gopal, MBBS
Fellow Physician
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background: Neonates with congenital diaphragmatic hernia (CDH) often have underlying pulmonary hypertension (PH) and cardiac dysfunction. Severity of PH and degree of ventricular dysfunction plays an important role in mortality and morbidity. These patients require varying levels of vasoactive medication support and are at high risk for adverse clinical outcomes. Need for multiple medications with high inotropic score (IS) and vasoactive inotropic score (VIS) has shown to have a predictive value in neonates undergoing congenital heart surgery and here we explore utilizing IS and VIS in patients with CDH.
Objective: Our objective was to investigate the utility of the inotropic score (IS) and vasoactive inotropic score (VIS) as tools to predict adverse clinical outcomes in CDH, and to correlate IS/VIS with postnatal echocardiographic variables.
Design/Methods: This was a retrospective chart review of 57 patients (Table 1) with CDH. We calculated the IS/VIS at 6-, 12-, 24-, 48- hours of life (HOL), on the day of CDH repair and 24- and 48- hours after repair. The association of these scores with postnatal echocardiographic markers was analyzed using Pearson’s correlation and linear regression, while logistic regression was used for binary outcomes, and Cox proportional hazards regression was used to assess associations with survival.
Results: Every one-unit increase in IS/VIS at 6 HOL was associated with a 13% increase in the odds of needing ECMO (p=0.034) and a 10.1% increase in risk of death (p=0.021) (Table 2). An increase in IS/VIS at 12-, 24- and 48- HOL was associated with posterior septal bowing in the first postnatal echocardiogram (p< 0.05 for all). We noted that left ventricle (LV) systolic function in the first postnatal echocardiogram was inversely related to IS (r= -0.281, p=0.036) and VIS (r= -0.288, p=0.031) calculated on the day of repair. Similarly, increase in IS (r= -0.307, p=0.024) and VIS (r= -0.285, p=0.037) on the day of repair was associated with decreased LV function on the post-repair echocardiogram (Table 3).
Conclusion(s): This study showed a significant association between IS/VIS obtained at various time points with clinical outcomes and echocardiographic findings in CDH, which can help guide prognosis and management in this patient population.