Neonatal Infectious Diseases/Immunology
Neonatal Infectious Diseases/Immunology 6
464 - Evaluation of Risks for Early-Onset Sepsis in Preterm Neonates Born After Preterm Premature Rupture of Membranes (PPROM)
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 464
Publication Number: 464.432
Publication Number: 464.432
Alexandria Sasaki, University of Pittsburgh School of Medicine, PIttsburgh, PA, United States; Danielle Browning, University of Pittsbrugh Medical Center, Pittsburgh, PA, United States; Eva Fandozzi, University of Pittsburgh School of Medicine, Pittsburgh, PA, United States; Anne-Marie Rick, University of Pittsburgh, Pittsburugh, PA, United States; Megli Christina, University of Pittsburgh School of Medicine, Pittsburgh, PA, United States
- AS
Alexandria Sasaki (she/her/hers)
Medical Student
University of Pittsburgh School of Medicine
PIttsburgh, Pennsylvania, United States
Presenting Author(s)
Background: Current management of suspected early-onset sepsis (EOS) for premature infants is empiric antibiotic therapy, though gestational age remains a strong predictor for EOS, there are few other risk stratification strategies that can be applied to preterm neonates. Neonates born to mothers diagnosed with preterm premature rupture of membranes (PPROM) are at high risk for early-onset sepsis, but the risk-benefit of antibiotic treatment is unclear as postnatal antibiotic exposure is associated with neonatal complications and rising antibiotic resistance.
Objective: Our objective is to evaluate a method of risk stratification for EOS for preterm neonates born after PPROM with the aim of reducing unnecessary antibiotic exposure.
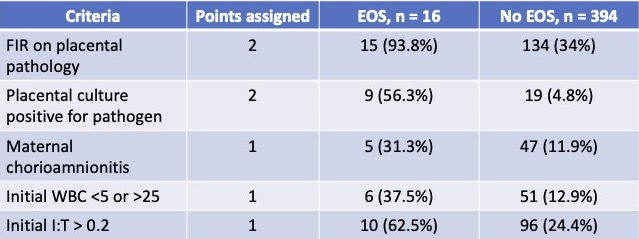
Design/Methods: This is a retrospective cohort study of neonates born to mothers diagnosed with PPROM identified by ICD-9 (658.10) and ICD-10 (O42.913) codes from 2015-2018. Neonates with congenital abnormalities, birth before 23 weeks, PPROM after 33 6/7, comfort measures only at delivery, absence of placental pathology, and absence of neonatal blood cultures were excluded. Data were stratified by presence of EOS. Five criteria associated with EOS were identified: fetal inflammatory response (FIR) on placental pathology, growth of pathogen on placental culture, maternal clinical chorioamnionitis diagnosis, initial neonatal WBC < 5 or > 25, and initial neonatal I:T ratio of > 0.2. Each of the criteria were assigned a score of 2, 2, 1, 1, and 1 points, respectively. Total scores of ≥ 2 were assigned high risk for EOS. Total scores of < two were determined as low risk for developing EOS.
Results: There were 410 neonates identified that met inclusion criteria; of those, 16 (3.9%) had culture-confirmed EOS. The proposed EOS risk stratification calculator was found to have a PPV of 9.9%and NPV of 100%. The sensitivity and specificity were determined to be 100% and 63%, respectively.
Conclusion(s): Among neonates born to mothers diagnosed with PPROM, our proposed EOS calculator had a high NPV of 100% and a sensitivity of 100%, which would greatly decrease the number of babies receiving unnecessary and potentially harmful antibiotics, while continuing to capture all those with true EOS. As PPROM accounts for 1/3 of all preterm delivery, efficient risk stratification could significantly decrease antibiotic usage in the NICU.