Back
Background: Asthma, pneumonia, and bronchiolitis are leading causes of childhood hospitalization. Clinicians face many barriers in adopting evidence-based guidelines, and this contributes to poor health outcomes for children hospitalized with these illnesses. The SIP trial (Simultaneously Implementing Pathways for Improving Asthma, Pneumonia, and Bronchiolitis Care for Hospitalized Children) is evaluating a high-efficiency clinical pathway intervention to improve guideline adherence.
Objective: Our objectives in this study were to prospectively identify barriers and facilitators of implementation in community/general hospitals.
Design/Methods: We recruited interdisciplinary participants from hospitals enrolled in the SIP trial. We designed an interview guide using the Consolidated Framework for Implementation Research. Individual interviews were recorded and transcribed, and qualitative analysis was done using constant comparative methods. Anticipated barriers were mapped to the Capability, Opportunity, Motivation, Behavior (COM-B) Framework, which was used to identify implementation facilitators.
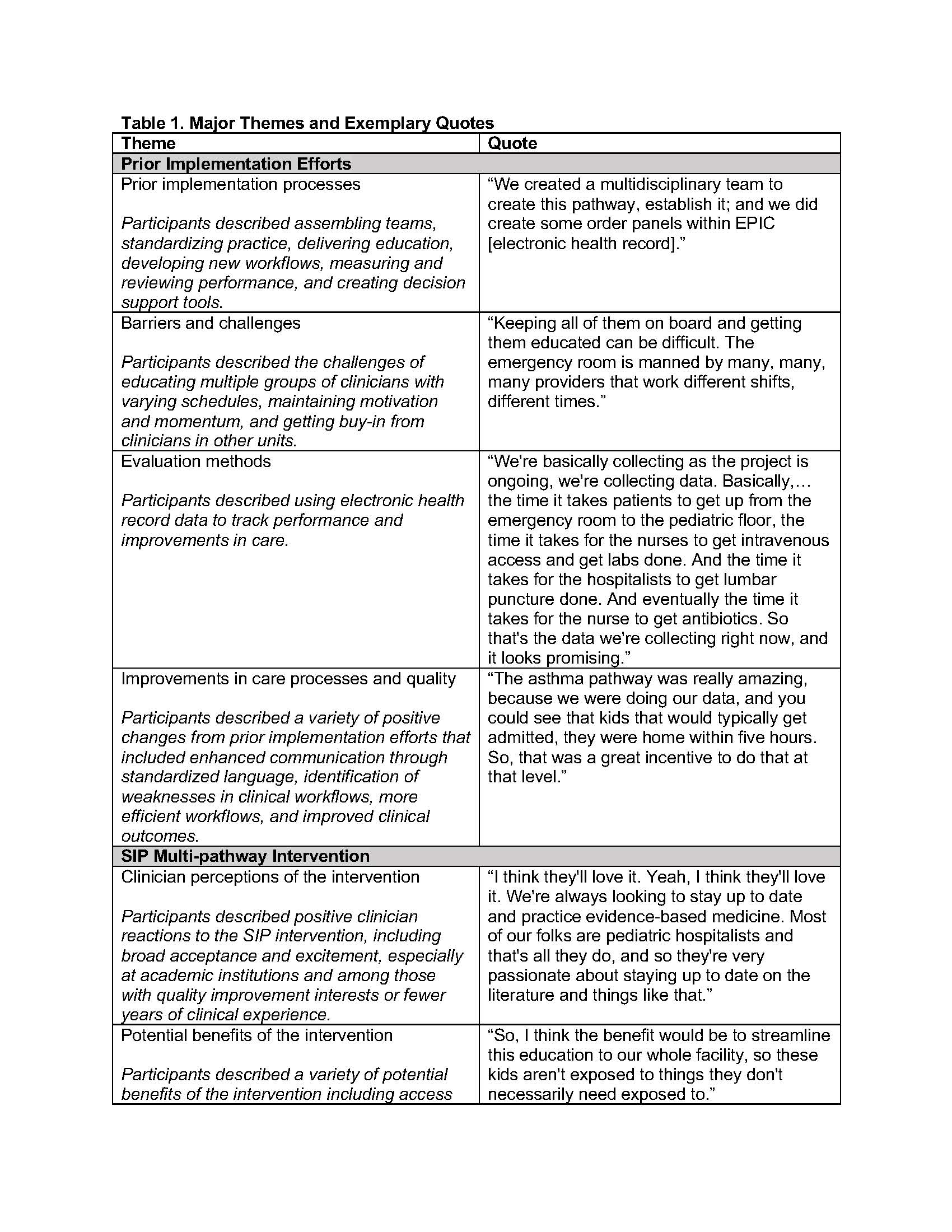
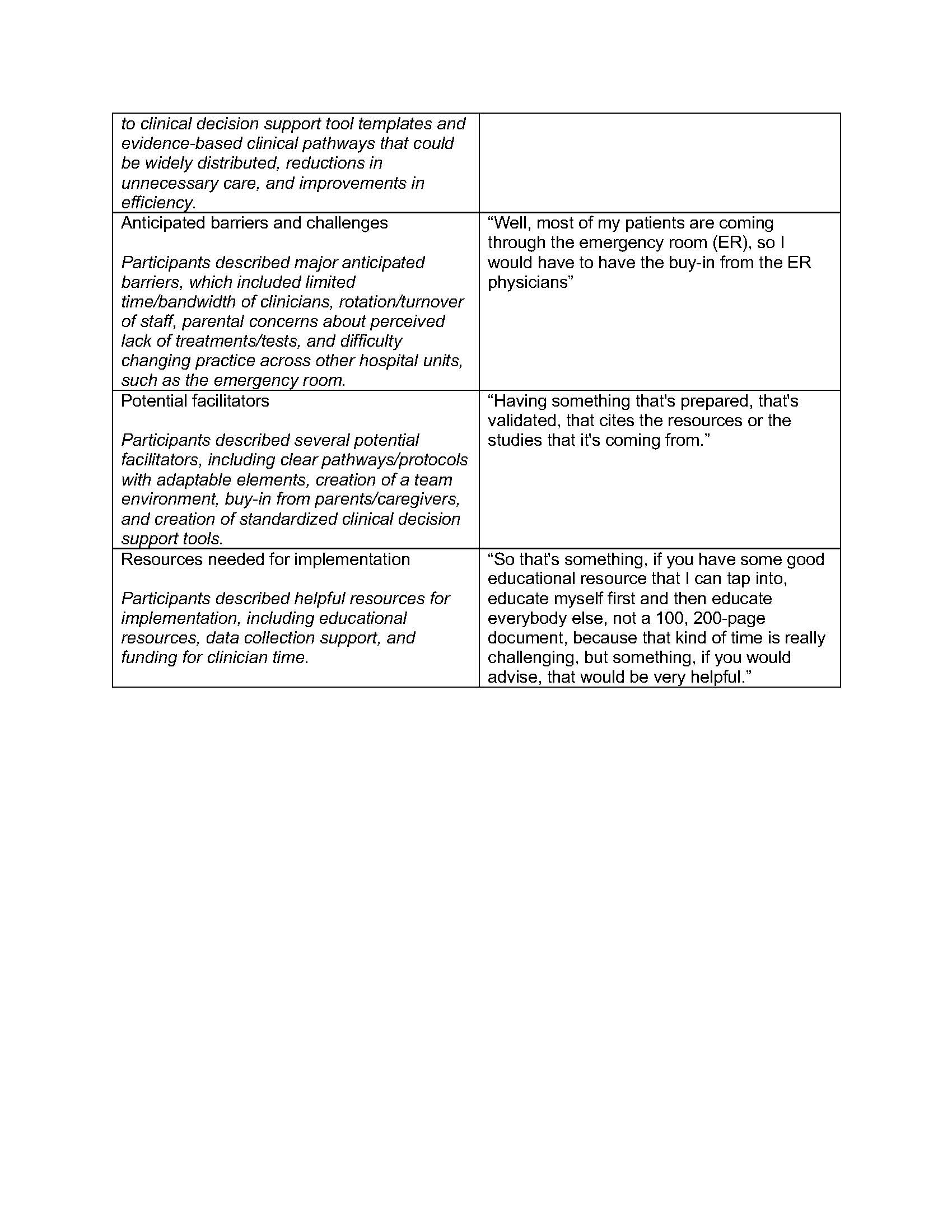
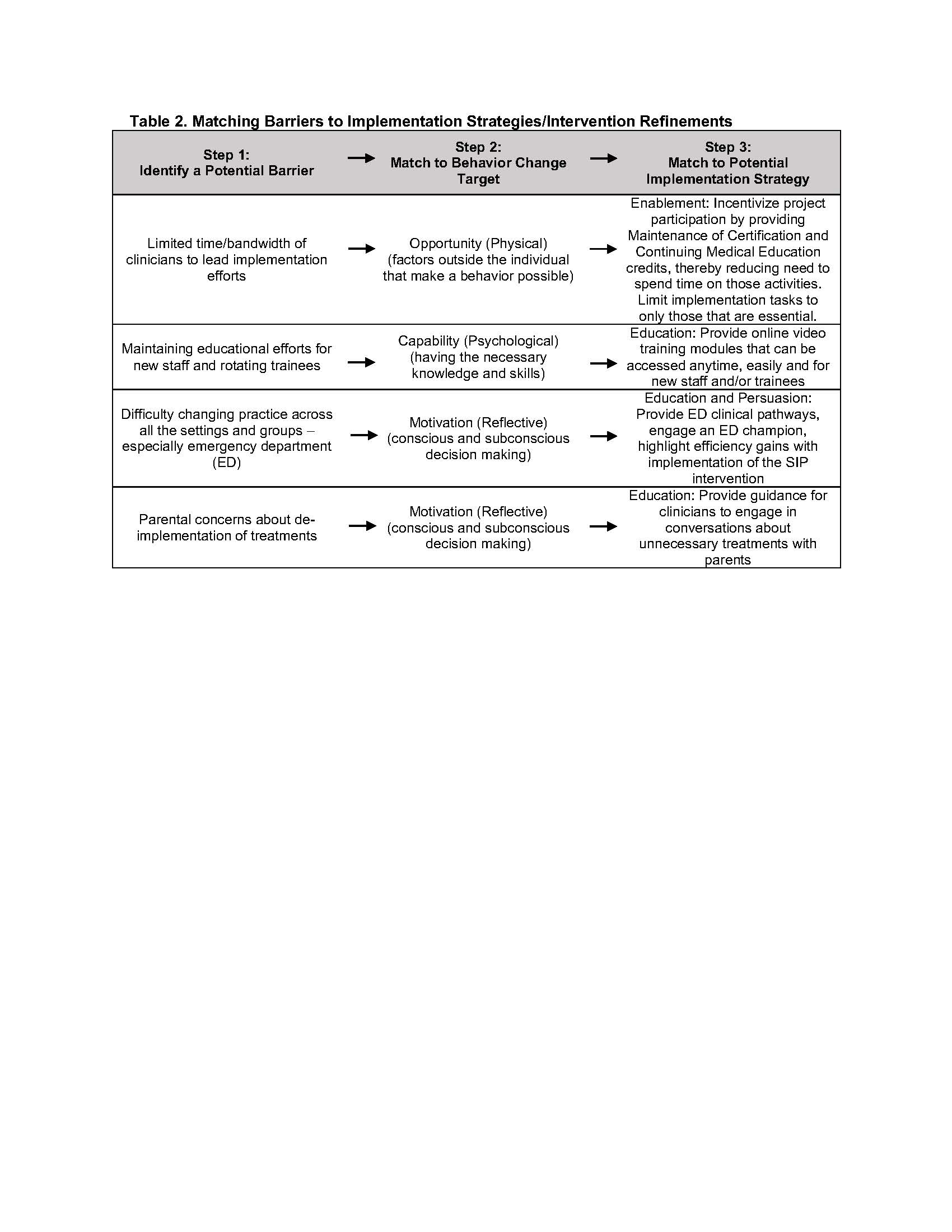
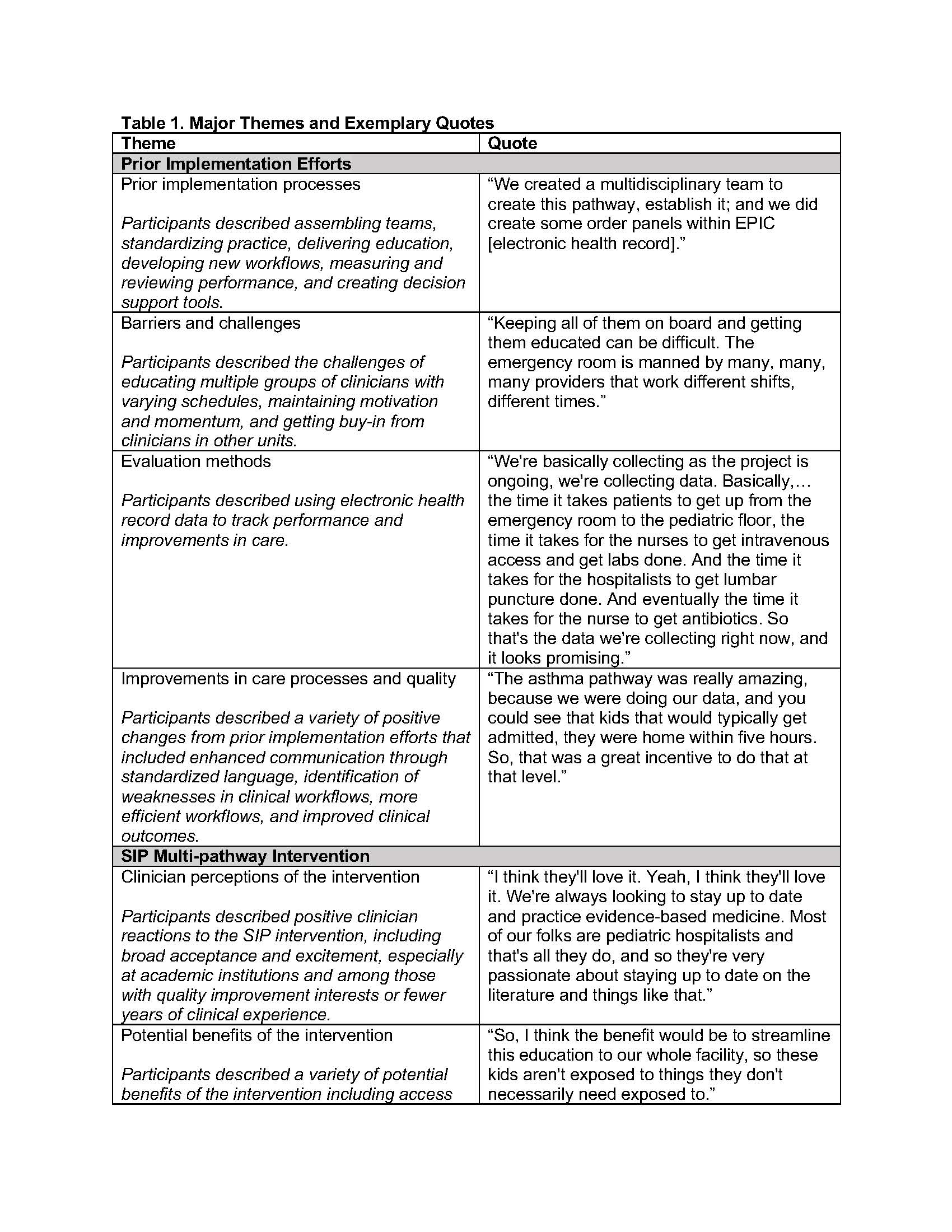
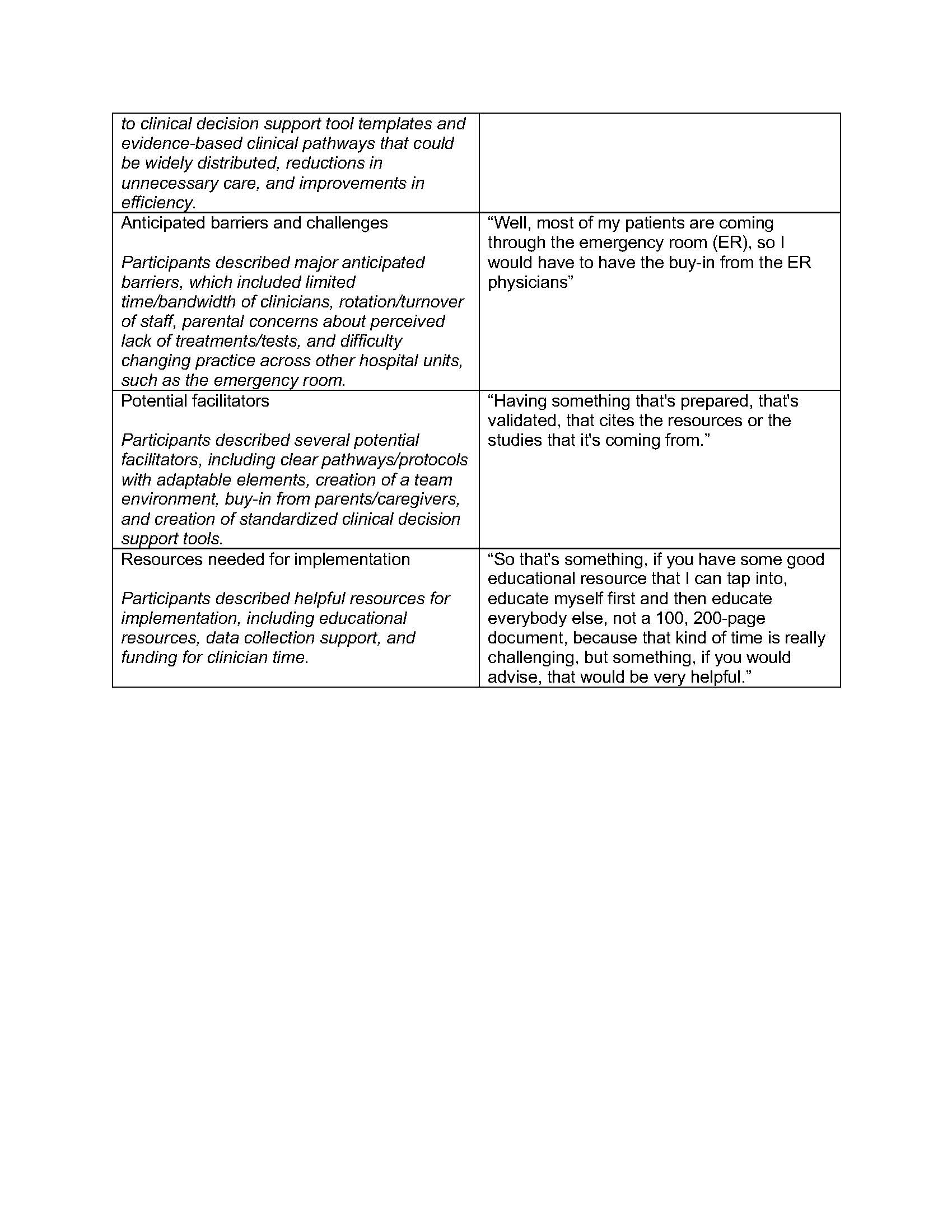
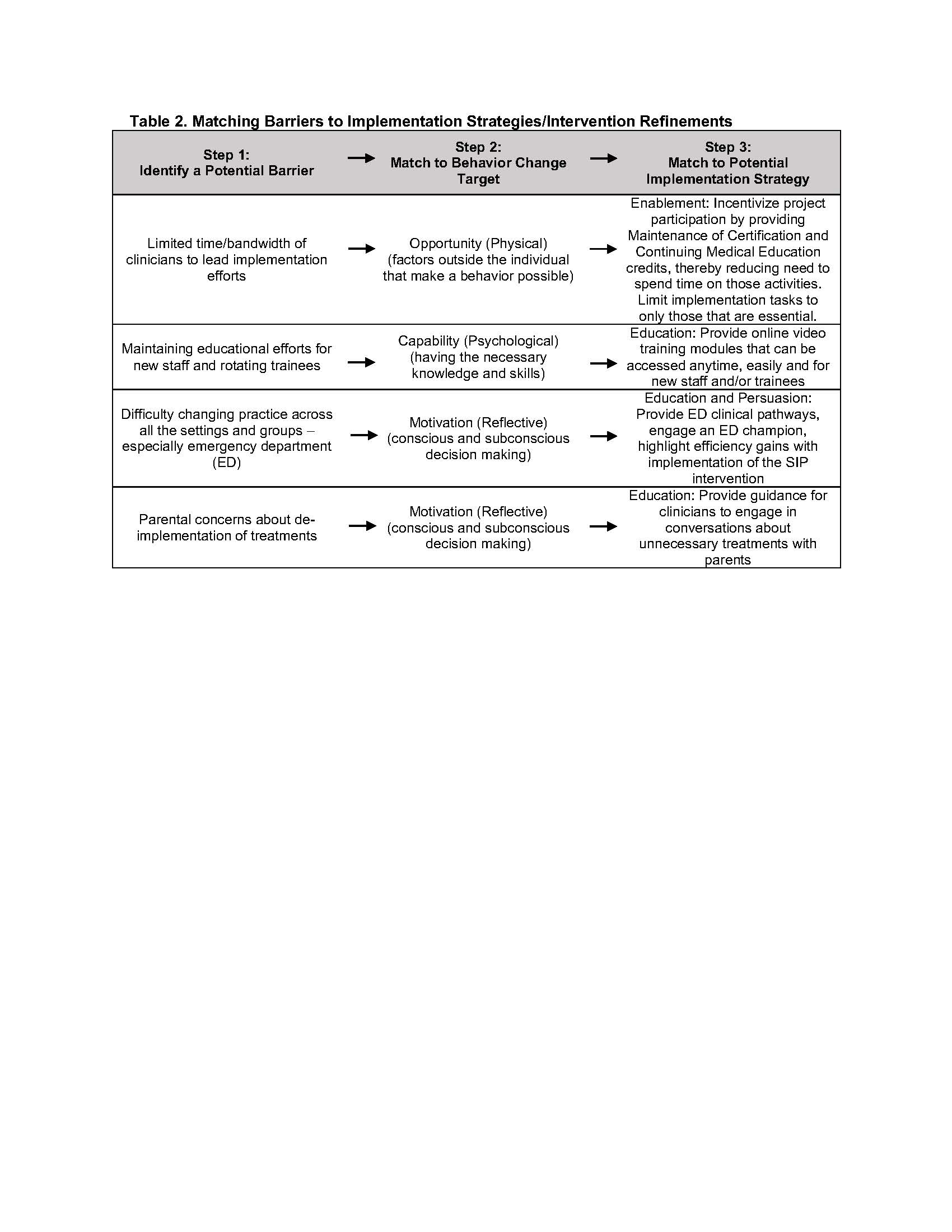
Results: Participants from 12 community hospitals across the US were interviewed (n=21). Major themes regarding prior implementation experiences included implementation processes, barriers/challenges, evaluation, and improvements in care quality (Table 1). Major themes regarding the upcoming pathway intervention included clinician perceptions, potential benefits, anticipated barriers, potential facilitators, and needed resources. We mapped barriers to additional potential facilitators using the COM-B framework (Table 2). To address limited time/bandwidth of clinicians, we will provide Maintenance of Certification credits. To address new staff and trainee turnover, we will provide easily accessible educational resources. To address difficulties in changing practice across other hospital settings/units, we will encourage early engagement of emergency department and primary care clinicians. To address potential parental concerns with de-implementation of treatments and tests, we will provide clinicians guidance on parent counseling.
Conclusion(s): We identified several potential facilitators of implementing a high-efficiency, multi-condition clinical pathway intervention in community hospitals. We also illustrate a prospective process for identifying implementation facilitators using implementation science frameworks.
Hospital Medicine: Hospital Medicine Quality Improvement
Hospital Medicine 7
766 - Barriers and Facilitators of High-Efficiency Clinical Pathway Implementation in Community Hospital Settings: A Qualitative Study
Monday, May 1, 2023
9:30 AM – 11:30 AM ET
Poster Number: 766
Publication Number: 766.416
Publication Number: 766.416
Simon Outram, UCSF, San Francisco, CA, United States; Sahar N.. Rooholamini, University of Washington School of Medicine, Seattle, WA, United States; Mansi Desai, UCSF, Burlingame, CA, United States; Yeelen Edwards, University of California, San Francisco, School of Medicine, San Anselmo, CA, United States; Clairissa Ja, University of California, Davis, San Francisco, CA, United States; Kayce Morton, CoxHealth, Springfield, MO, United States; Jordan Vaughan, UCSF Benioff Children's Hospital San Francisco, San Francisco, CA, United States; Judy Shaw, Larner College of Medicine,University of Vermont, S BURLINGTON, VT, United States; Ralph Gonzales, UCSF, San Francisco, CA, United States; Sunitha V. Kaiser, University of California, San Francisco, School of Medicine, San Francisco, CA, United States

Sunitha V. Kaiser, MD, MSc (she/her/hers)
Associate Professor
University of California, San Francisco, School of Medicine
San Francisco, California, United States
Presenting Author(s)
Background: Asthma, pneumonia, and bronchiolitis are leading causes of childhood hospitalization. Clinicians face many barriers in adopting evidence-based guidelines, and this contributes to poor health outcomes for children hospitalized with these illnesses. The SIP trial (Simultaneously Implementing Pathways for Improving Asthma, Pneumonia, and Bronchiolitis Care for Hospitalized Children) is evaluating a high-efficiency clinical pathway intervention to improve guideline adherence.
Objective: Our objectives in this study were to prospectively identify barriers and facilitators of implementation in community/general hospitals.
Design/Methods: We recruited interdisciplinary participants from hospitals enrolled in the SIP trial. We designed an interview guide using the Consolidated Framework for Implementation Research. Individual interviews were recorded and transcribed, and qualitative analysis was done using constant comparative methods. Anticipated barriers were mapped to the Capability, Opportunity, Motivation, Behavior (COM-B) Framework, which was used to identify implementation facilitators.
Results: Participants from 12 community hospitals across the US were interviewed (n=21). Major themes regarding prior implementation experiences included implementation processes, barriers/challenges, evaluation, and improvements in care quality (Table 1). Major themes regarding the upcoming pathway intervention included clinician perceptions, potential benefits, anticipated barriers, potential facilitators, and needed resources. We mapped barriers to additional potential facilitators using the COM-B framework (Table 2). To address limited time/bandwidth of clinicians, we will provide Maintenance of Certification credits. To address new staff and trainee turnover, we will provide easily accessible educational resources. To address difficulties in changing practice across other hospital settings/units, we will encourage early engagement of emergency department and primary care clinicians. To address potential parental concerns with de-implementation of treatments and tests, we will provide clinicians guidance on parent counseling.
Conclusion(s): We identified several potential facilitators of implementing a high-efficiency, multi-condition clinical pathway intervention in community hospitals. We also illustrate a prospective process for identifying implementation facilitators using implementation science frameworks.