Quality Improvement/Patient Safety: All Areas
QI 5: Quality Measures, Family Centered & Inpatient QI
248 - Optimizing Family Centered Rounds: A Trainee-Led Initiative Back to the Bedside
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 248
Publication Number: 248.451
Publication Number: 248.451
Colin J. Crilly, Children's Hospital of Philadelphia, Philadelphia, PA, United States; John P. Simmons, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Jeremy M. Jones, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Kim Tran Lopez, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Kristin Maletsky, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Katherine Pumphrey, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Beatriz Milet Letelier, The Children’s Hospital of Philadelphia, Philadelphia, PA, United States; Jessica Hart, Childrens Hospital of Philadelphia, Philadelphia, PA, United States

Preston Simmons, MD (he/him/his)
Resident Physician
Childrens Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: The American Academy of Pediatrics describes family centered rounding (FCR) as the standard rounding practice in pediatrics, but barriers such as large rounding teams and increased patient volumes can limit bedside rounding. Pediatric trainees at a large, free-standing children’s hospital had previously examined the state of FCR at their institution in the early aftermath of the COVID-19 pandemic and found that FCR happened infrequently despite patient, family, nursing, and physician interest in the practice.
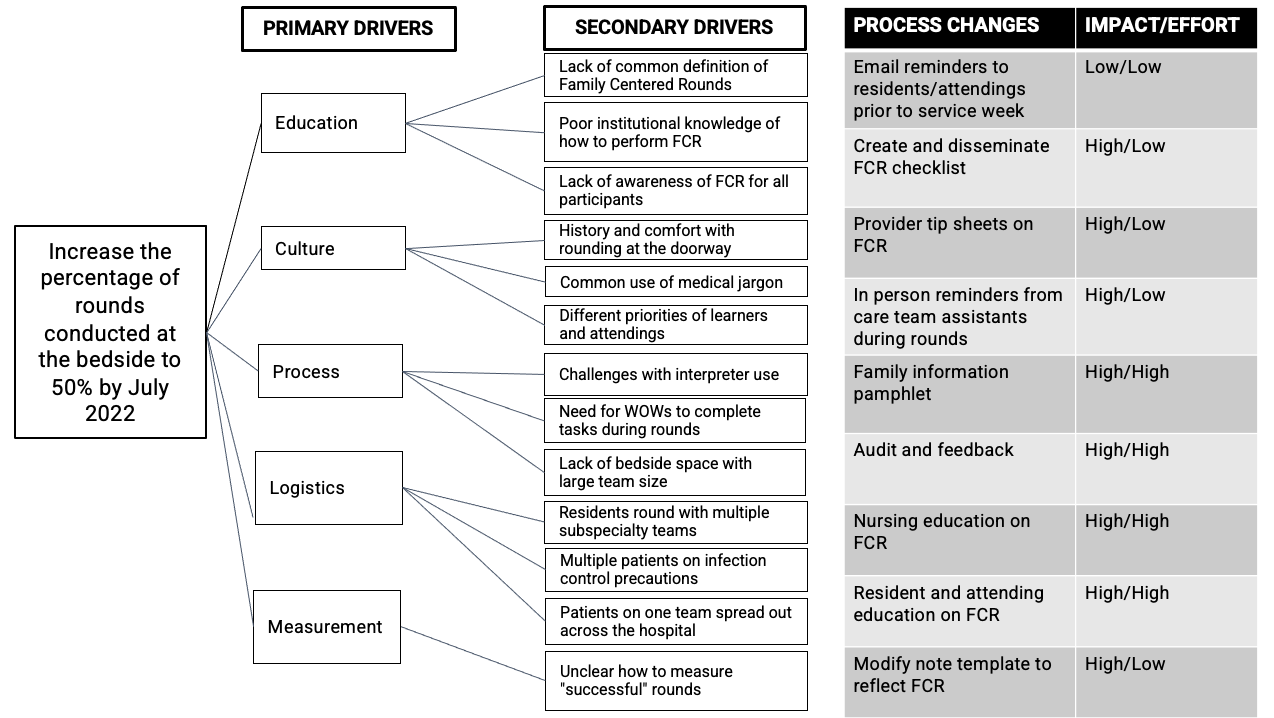
Objective: Trainees aimed to: 1) increase bedside rounding from a pre-intervention baseline of 17% to 50% by 7/1/2022 on a resident inpatient general pediatrics (GP) team, 2) address barriers to implementation using quality improvement (QI) methodologies, and 3) demonstrate sustained improvement in FCR on the pilot team over nine months.
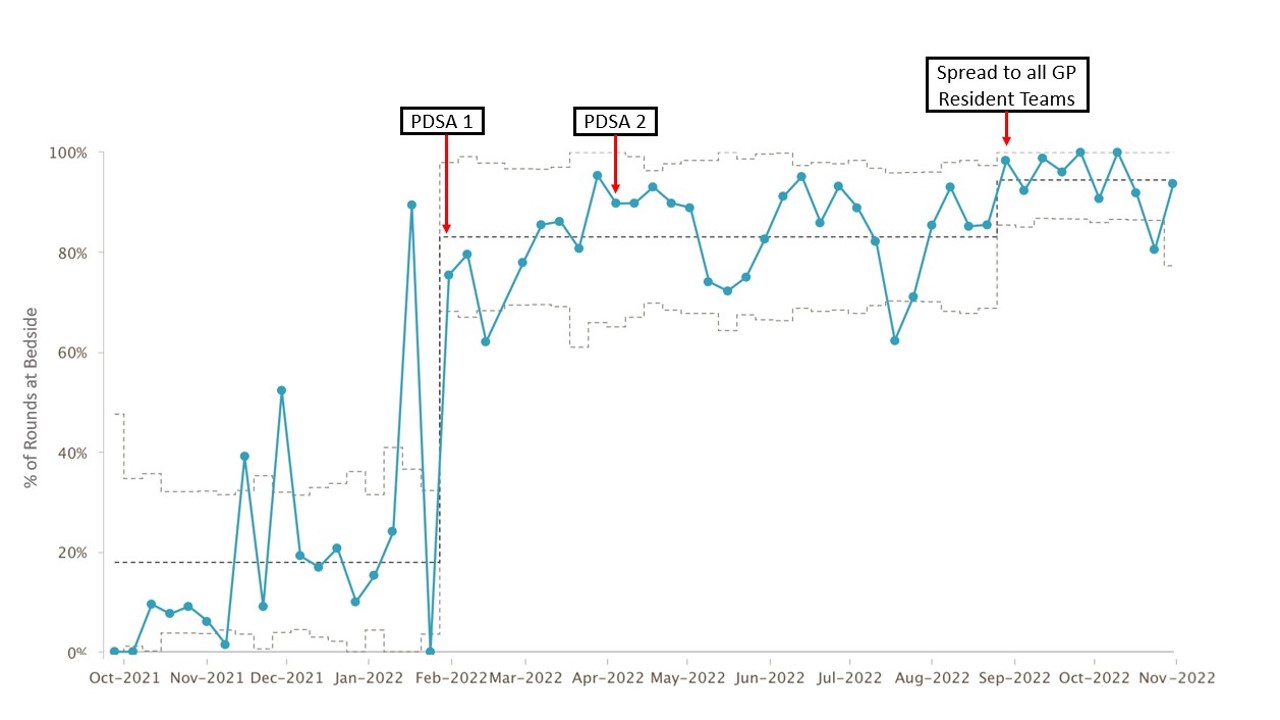
Design/Methods: The Model for Improvement was used to understand the process, barriers, and drivers of FCR (Figure 1). The initial PDSA cycle included electronic communication to oncoming residents and attendings providing the FCR operational definition, a guiding checklist, and an implementation tip sheet. Later PDSA cycles included establishing a nursing rounding order and spreading to remaining GP teams. Baseline rounding data from the pilot inpatient GP team was collected from 10/1/2021-11/30/2022. The primary outcome measure was percentage of rounds occurring at the patient bedsides. Nursing and family presence on rounds were process measures. Balancing measures included rounding time and surveyed resident and attending perception of FCR.
Results: Following the initial PDSA cycle, percentage of bedside rounds increased from 17% to 83% and family presence on rounds increased from 67% to 98%. Nursing presence was unchanged from a baseline of 75%. Bedside rounding increased further to 94% with subsequent PDSA cycles (Figure 2). Rounding time increased from 130 minutes to 169 minutes. Surveyed attendings and residents reported benefits in workflow, communication, and education.
Conclusion(s): A trainee-led team successfully initiated and sustained an improvement in bedside rounding on a GP service. Despite the small increase in rounding time, workflow reportedly improved. Initial uptake of the intervention was dramatic, with rapid culture change in part due to trainee engagement. Bedside rounding was notably used as a proxy measure for FCR, though it does not directly measure the quality of FCR performed. Ongoing challenges include perceived restrictions with patients under infection precautions and decreased stakeholder engagement during periods of high census.