Neonatal Neurology: Clinical Research
Neonatal Neurology 6: Clinical 6
128 - Pre-Vent study: Relationship between neonatal hypoxemic event duration and neuromotor impairment in infants born extremely preterm
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 128
Publication Number: 128.338
Publication Number: 128.338
Erin Lonergan, Ann & Robert H. Lurie Children's Hospital of Chicago, Palos Heights, IL, United States; Lynn D. Boswell, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Casey Rand, lurie childrens hospital and stanley manne research center, Chicago, IL, United States; Narayanan Krishnamurthi, Lurie Children's Hospital, Chicago, IL, United States; Ryne Estabrook, University of Illinois at Chicago, Chicago, IL, United States; Aaron Hamvas, Lurie Children's Hospital / Northwestern University, Chicago, IL, United States; Douglas E. Lake, University of Virginia, Charlottesville, VA, United States; J. Randall Moorman, University of Virginia School of Medicine, Charlottesville, VA, United States; Debra E. Weese-Mayer, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Raye-Ann deRegnier, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States

Erin Lonergan, MS, RRT (she/her/hers)
Lead Clinical Research Coordinator
Ann & Robert H. Lurie Children's Hospital of Chicago
Palos Heights, Illinois, United States
Presenting Author(s)
Background: Intermittent hypoxemia occurs commonly in infants born extremely preterm. Recent retrospective studies suggest a relationship between the duration of neonatal hypoxemic events and neuromotor impairments. Prospective studies quantifying the timing and duration of hypoxemic events and neuromotor impairments are necessary.
Objective: To prospectively examine the duration of hypoxemic events during the first eight weeks of life and the relationship to neuromotor impairment at 6-15 months corrected age (CA) in infants born extremely preterm.
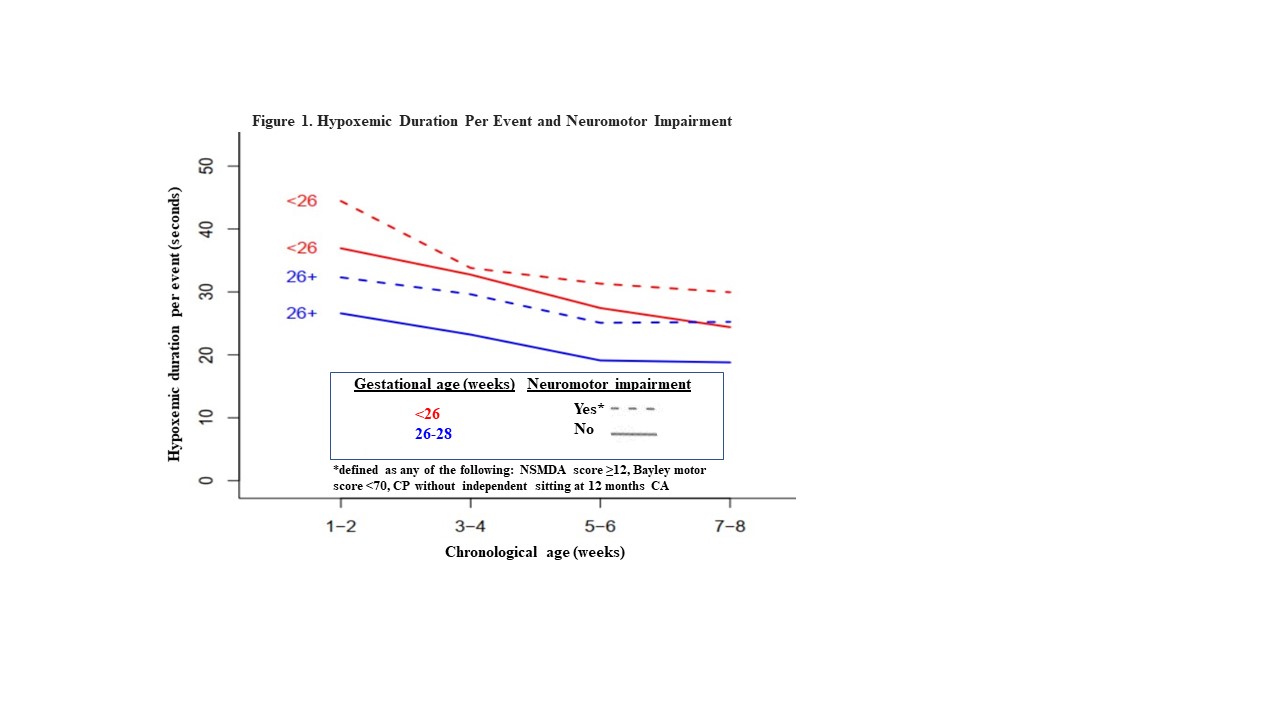
Design/Methods: The cohort included 98 infants born between 23 and 286/7 weeks gestational age (GA). Continuous SpO2 data were captured by the bedside monitor up to eight weeks after birth. The Neuro-Sensory Motor Developmental Assessment (NSMDA), Bayley Scales of Infant and Toddler Development third or fourth edition (Bayley®-III, BayleyTM-4), and cerebral palsy (CP) diagnoses were captured at 6-15 months CA. Neuromotor impairments were defined as any of the following: NSMDA score ≥12, Bayley motor score < 70, CP without independent sitting at 12 months CA. Duration per event (dpe) of hypoxemia (< 80% SpO2, 10-300 seconds) over time (grouped by fortnight) was associated with GA (< 26 wks vs. 26-286/7wks) and neuromotor outcomes. Mixed effect modeling was used to account for the clustering inherent to our longitudinal data.
Results: (Figure 1) The average dpe of hypoxemia decreased over the first eight postnatal weeks (p< .001). Average dpe of hypoxemia was longer in infants with GA < 26 weeks compared to infants with GA 26-286/7 weeks (p< .001). Infants with neuromotor impairments had longer average dpe than infants without impairments (p< .01) for both GA groups.
Conclusion(s): In both GA groups, dpe of hypoxemia decreased over the first eight postnatal weeks. Longer events were observed in infants with neuromotor impairment, regardless of GA. Longer follow up and larger cohorts are needed, but if confirmed, specific interventions to reduce the duration of hypoxemic events may lead to improvements in rates of developmental impairments in infants with extreme prematurity.
Funding: NIH U01HL133704 & U01HL133708.