Neonatal Neurology: Clinical Research
Neonatal Neurology 6: Clinical 6
125 - Impact Of A Standardized Neuroimaging AND THErapeutic Considerations (SNATHEC) Algorithm On Short-Term Outcomes Of Preterm Infants At Risk For Intraventricular Hemorrhage
Publication Number: 125.338

Heather Bruckman, DNP, NNP (she/her/hers)
NeuroNICU Team Lead NNP
Riley Hospital for Children at Indiana University Health
Indianapolis, Indiana, United States
Presenting Author(s)
Background: Head ultrasound (HUS) is the standard of care for monitoring preterm infants at risk for intraventricular hemorrhage (IVH) and subsequent post hemorrhagic hydrocephalus (PHH), both common precursors of neurodevelopmental impairments (NDI). Early serial screening with HUS benefits infants at risk for NDI as identification of issues can be followed by early intervention. However, there is no consensus on frequency or timing of serial neuroimaging exams for preterm infants who develop IVH and PHH.
Objective:
Our study objective was to evaluate the impact of a “Standardized Neuroimaging And THErapeutic Considerations” (SNATHEC) algorithm on short term outcomes of preterm infants at risk for IVH.
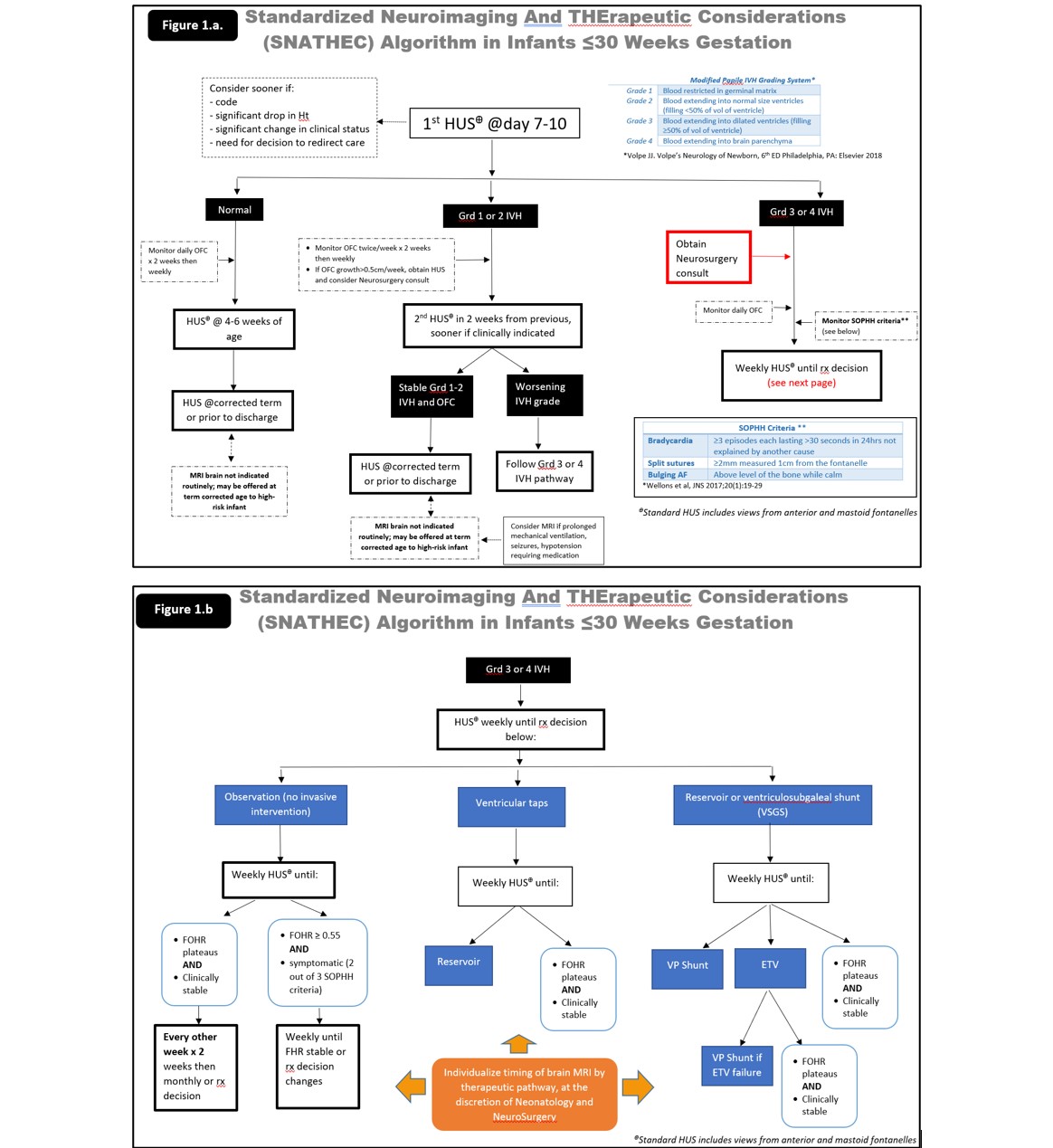
Design/Methods: This was a single center, quasi-experimental study of infants less than 30 weeks gestation at risk for IVH and PHH. A SNATHEC algorithm was developed by a multidisciplinary team with neonatology, neurosurgery and neurology input and was implemented in January 2021 (Figure 1). Eligible infants admitted January-December 2020 comprised the Control group and infants admitted January-December 2021 comprised the SNATHEC group.
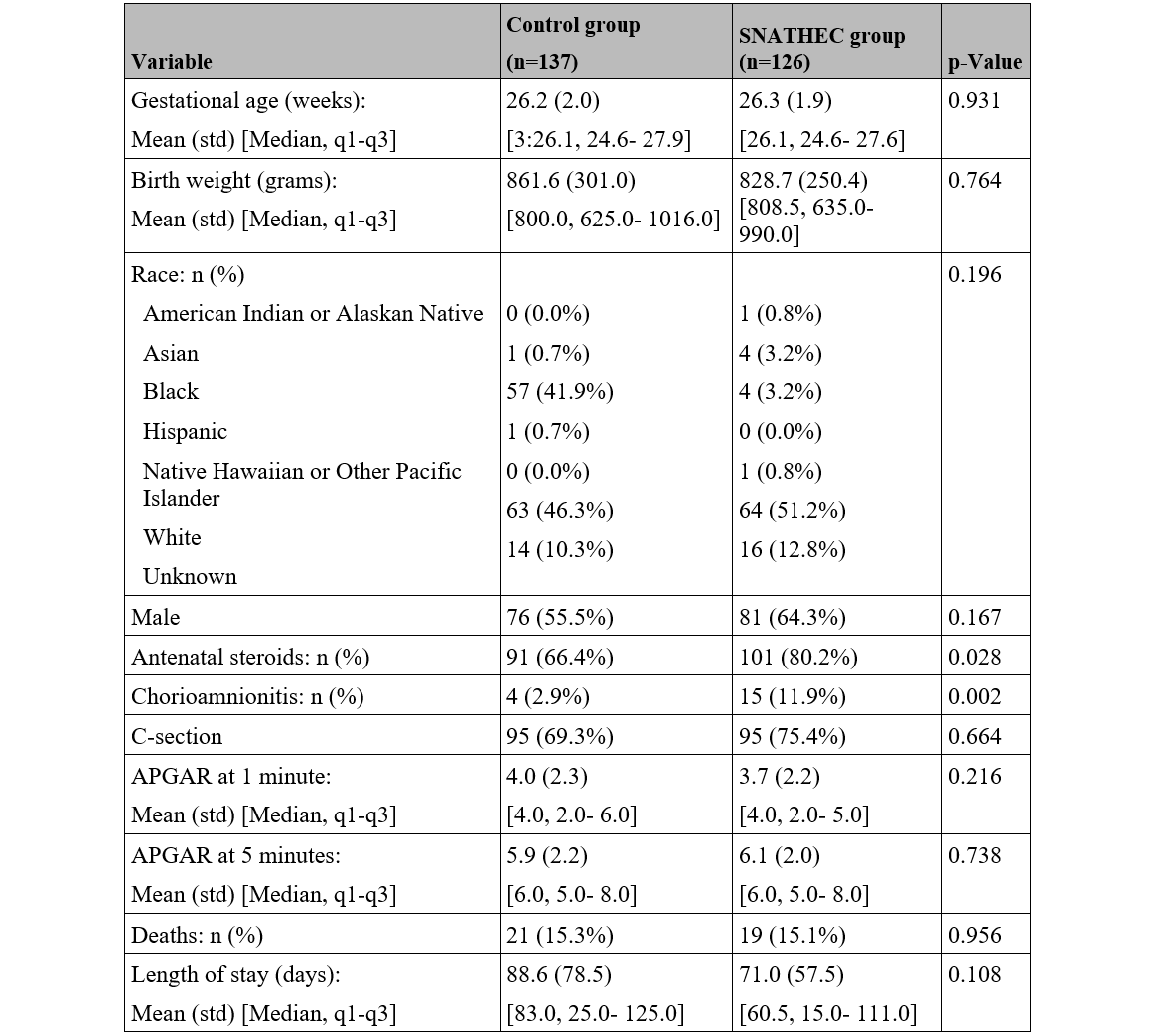
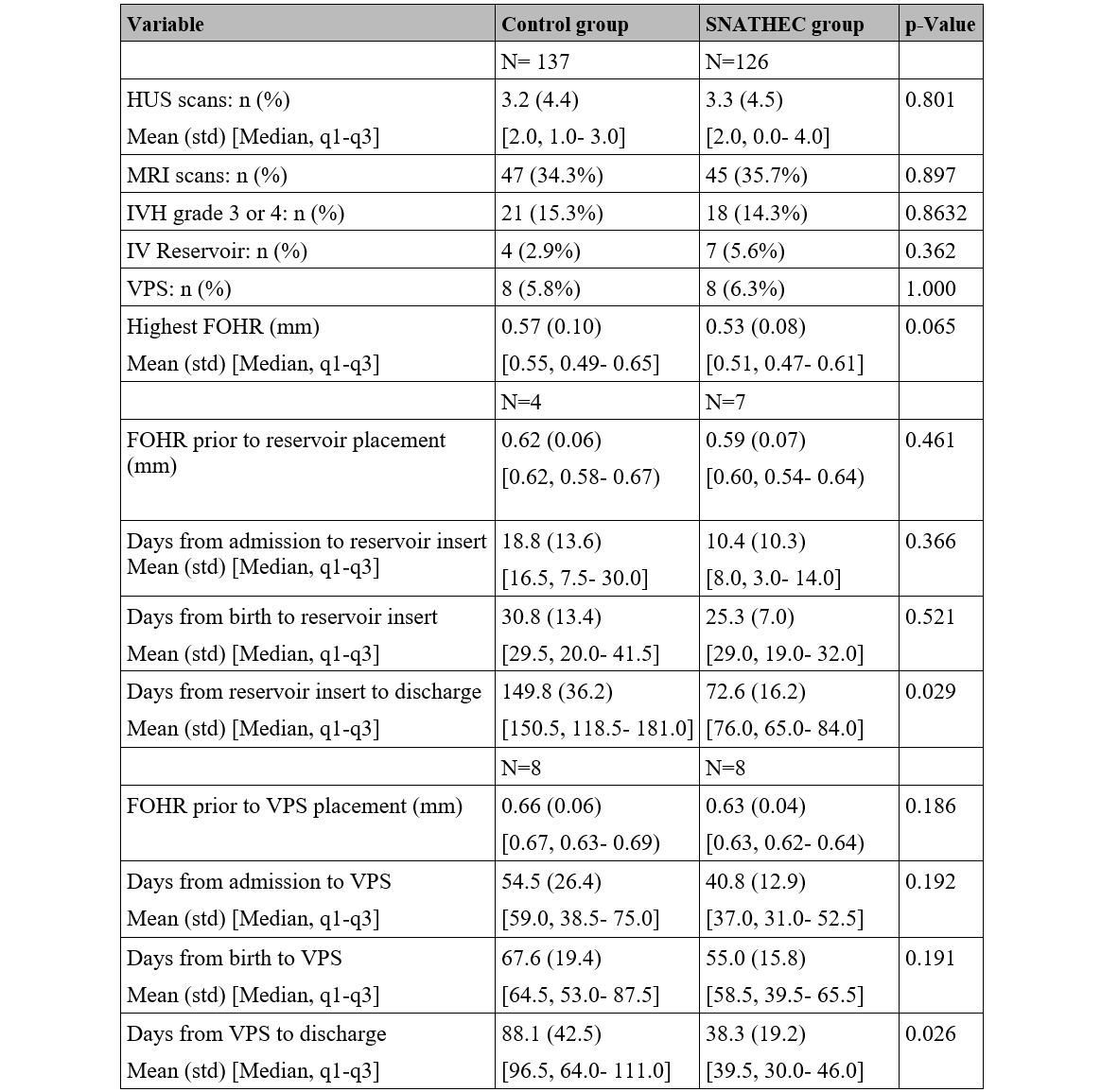
Results: There were 263 infants included in the study, of which 137 in the Control group and 126 in the SNATHEC group. Baseline characteristics, shown in Table 1, were similar between study groups with exception of chorioamnionitis, which was significantly higher in the Control group (p=0.02), and antenatal steroid use, which was significantly higher in the SNATHEC group (p=0.03). There were 8 infants who required VPS placement in the Control group, of which 4 (50%) had a preceding intraventricular reservoir. Similarly, there were 8 infants who required a VPS placement in the SNATHEC group, of which 7 (87.5%) had a preceding intraventricular reservoir. Although there was no significant difference in length of stay (LOS) between study groups, infants in the SNATHEC group who required device placement (reservoir and ventriculoperitoneal shunt) had significantly shorter LOS from the time of device placement to discharge compared to the Control group (reservoir: 76 [65, 84] versus 150.5 [118.5, 181], p=0.03; ventriculoperitoneal shunt: 39.5 [30,46] versus 96.5 [64,111], p=0.03; Table 2). There was no significant difference with respect to the number of neuroimaging scans obtained.
Conclusion(s): Successful implementation of the SNATHEC algorithm in high-risk preterm infants was associated with shorter hospital stays for infants who required intraventricular device placement without increase in neuroimaging frequency and its associated costs.