General Pediatrics: Primary Care/Prevention
General Pediatrics 5
390 - Improving Resident Knowledge and Comfortability in Diagnosing Dermatologic Conditions in Patients with Skin of Color
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 390
Publication Number: 390.314
Publication Number: 390.314
Valerie Vernot, Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo, Buffalo, NY, United States; Jordan Hart, Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo, Buffalo, NY, United States; Lisa Samuels-Cox, Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo, Buffalo, NY, United States; Victoria M. Sarata, John R. Oishei Children's Hospital, Buffalo, NY, United States; Alanna N. Grafius, Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo, Buffalo, NY, United States; Robert R. welliver, Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo, East Amherst, NY, United States; Mary Emborsky, University at Buffalo, Buffalo, NY, United States

Jordan Hart, MD (she/her/hers)
Resident
Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo
Buffalo, New York, United States
Presenting Author(s)
Background: There has been a significant effort to bring forth and address the gap in society’s deep rooted racial differences. Historically, medical training lacks substantial representation of skin of color (SoC) in textbooks, lesson plans, and learning objectives. As a result, the lack of representation in educational materials, especially for current and future resident physicians, creates an unfair disparity in patients of color leading to delayed diagnosis, treatment and ultimately a decreased quality of care.
Objective: Address the discomfort, bias, and lack of knowledge in diagnosing and treating dermatologic conditions in SoC by resident physicians. Our goal is to improve both level of comfort and accuracy in diagnosis by 50% when treating non-white skin within one year of implementing our curriculum.
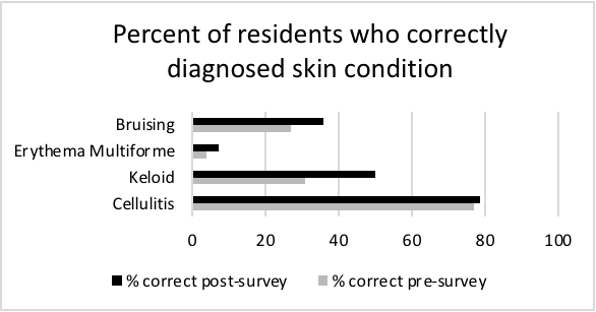
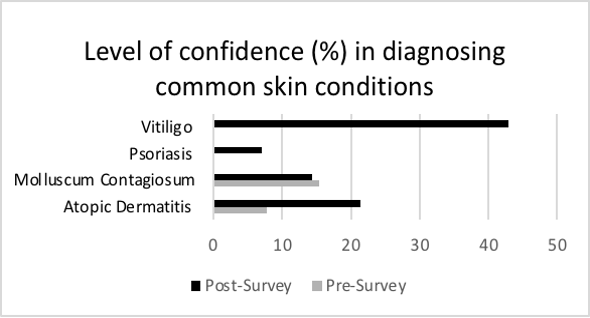
Design/Methods: A survey was distributed to pediatric residents at John R. Oishei Children's Hospital in Buffalo, New York. Using a Likert Scale, we measured the level of comfort in diagnosing and treating common conditions in SoC. We then measured their ability to correctly diagnose skin conditions using color photos. After which, we provided a series of resident-led lectures and summary documents encompassing these previously assessed knowledge deficits. The same survey was redistributed to the residents after completion of the course. Data showed a change in both subjective and objective measurements for comfort level and knowledge in diagnosis, respectively (Figure 1&2).
Results: Initially, 26 residents responded to the pre-survey; 76.9% of the respondents reported a lack of adequate SoC education during medical school and in residency, and only 7.7% reported feeling confident identifying dermatologic conditions in SoC. After the first educational cycle, 42.9% of respondents (n=14) felt confident in recognizing these conditions and there was an overall increase in percent of correct diagnosis (Figures 1&2).
Conclusion(s): Our curriculum exposed residents to various dermatologic conditions in SoC and improved confidence as well as accuracy in diagnosis. In our upcoming PDSA cycles, we will incorporate weekly image quizzes into didactic lectures and provide a review handbook to increase education and participation among residents. We continue to strive to increase awareness and education with the ultimate goal of providing better care and improved management of our diverse pediatric population.