Neonatal Neurology: Clinical Research
Neonatal Neurology 4: Clinical 4
94 - The prognostic capacity of an automated quantitative measure of EEG monitoring after neonatal encephalopathy
Publication Number: 94.336

Micheline Lagacé, MD, FRCPC (she/her/hers)
Neonatal neurology fellow, Clinician investigator program
University of British Columbia Faculty of Medicine
Toronto, Ontario, Canada
Presenting Author(s)
Background:
Assessing early brain recovery with EEG supports prognostication after neonatal encephalopathy. Brain State of the Newborn (BSN) is a recently developed automated measure of EEG background activity, which translates EEG into a continuous score from 0 to 100, and can be displayed as a trend on bedside monitors.
Objective:
To assess the capacity of BSN to predict neurodevelopmental outcomes in neonatal encephalopathy.
Design/Methods:
From an out-born center, 100 newborns ≥36 weeks PMA with neonatal encephalopathy were recruited within 6 hours of life and monitored with a long-term EEG for at least 48 hours. The BSN was calculated off-line for every minute of EEG recording, using four EEG channels. The neurodevelopmental evaluation was done at 18 months using the Bayley-III. Poor outcome was defined by death and low composite scores on the Bayley-III, with the conservative threshold being ≤70 and the inclusive threshold being ≤85. Poor overall outcome was defined as death or poor outcome in at least one Bayley-III composite score. Receiver operating characteristic (ROC) and likelihood ratio (LR) curves at specific ages were used to assess the capacity of BSN to predict outcomes.
Results:
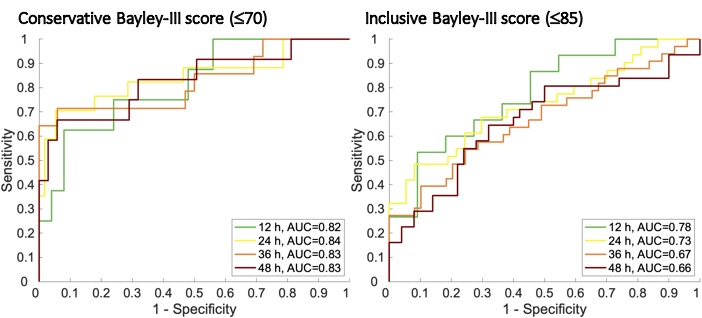
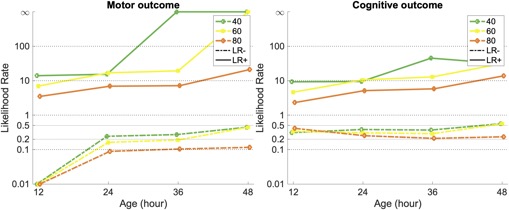
The final analyses included 92 infants, 61% males, born at 39.6±1.3 weeks PMA, with umbilical artery pH 7.00±0.17. There were 9 neonatal deaths, and 1 infant died from sudden infant death syndrome after the neonatal period. Poor outcomes were documented in 21 infants (23%) using conservative Bayley-III cut-offs, and in 40 infants (44%) using inclusive cut-offs. Poor outcomes were better predicted using the conservative instead of the inclusive Bayley-III cut-offs, with BSN during the first 24 hours of life best predicting poor outcome at 18 months (AUC=0.84; Figure 1). Using the conservative cut-offs for developmental domains, BSN during the first 24 hours of life best predicted motor (AUC=0.97) and language (AUC=0.82) outcomes, while cognitive outcomes were best predicted by BSN during the first 36 hours of life (AUC=0.90). Temporal evolution of prognostication by BSN is emphasized when using specific BSN thresholds to calculate LRs (Figure 2). Regarding poor motor outcomes with conservative cut-offs, a BSN score of 60 at 24h of life corresponds to a negative LR of 0.08 and a positive LR of 16.16 (Figure 2).
Conclusion(s):
BSN is a promising open-access algorithm for early interpretation of EEG background in patient with neonatal encephalopathy. Compared to amplitude-integrated EEG and EEG, BSN offers a fully automated and quantitative information for early brain monitoring to support prognostication as early as 24h.