Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 3: Physiology 2 and Clinical Outcomes
343 - Tracking Lung Volume During Total Liquid Ventilation in Newborn Piglets
Publication Number: 343.346

Alexandru Panaitescu (he/him/his)
MD-MSc Candidate
Universite de Sherbrooke Faculty of Medicine
Sherbrooke, Quebec, Canada
Presenting Author(s)
Background:
Total liquid ventilation (TLV), using liquid perflubron, could be an alternative for early respiratory support of nano-preterm infants. However, due to the greater compliance of the tracheobronchial tree in immature subjects, airway tendency to collapse during active expiration can lead to progressive accumulation of perflubron and volutrauma.
Objective:
Our objective was to demonstrate the possibility of maintaining stable intrapulmonary perflubron volumes during TLV using our current ventilation approach.
Design/Methods:
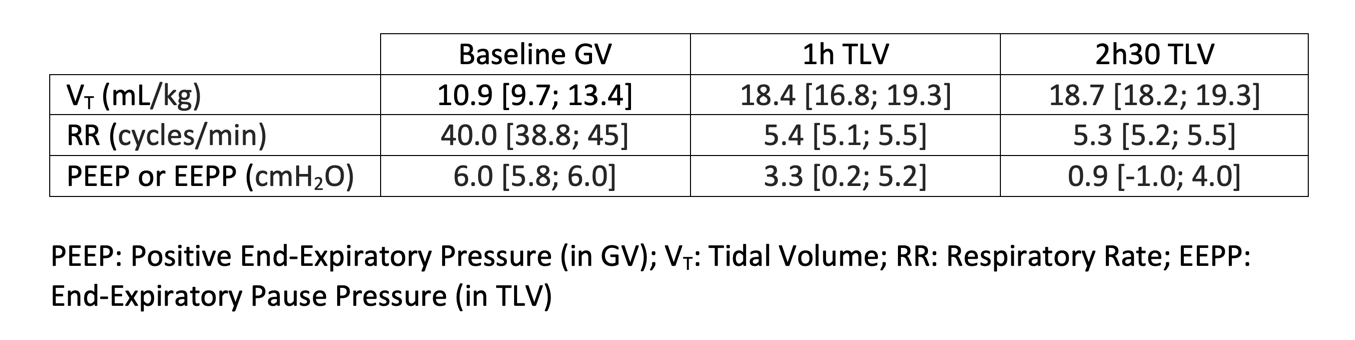
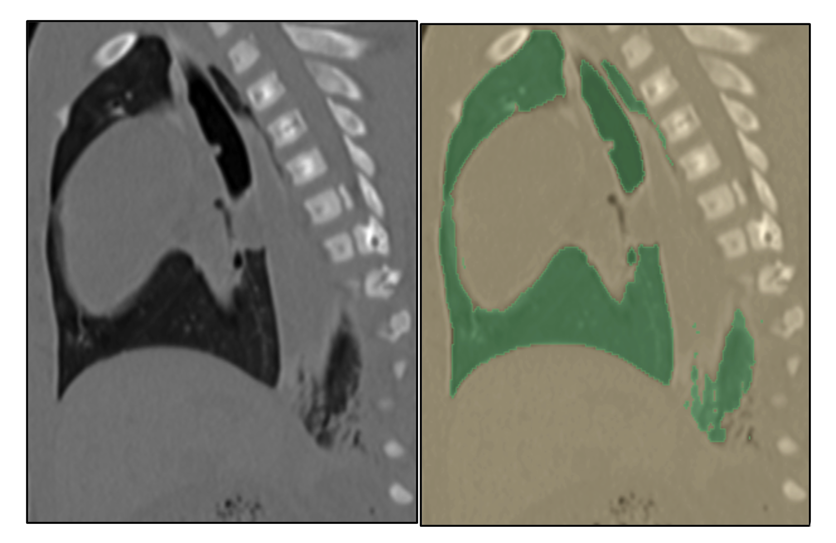
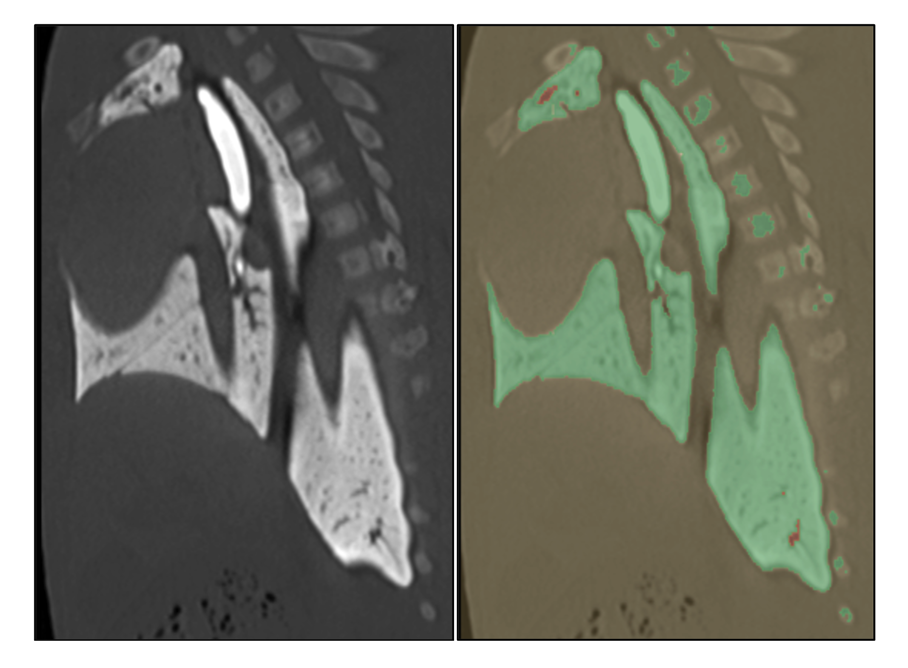
Six newborn piglets aged 3.5 [2.75; 5.25] days and weighing 1.93 [1.80; 2.09] kg were instrumented (tracheotomy, jugular and carotid catheters) under general anesthesia. At baseline, during conventional mechanical gas ventilation, a CT scan was performed to determine total lung volume at end-expiration. The subjects then underwent a 3-hour total liquid ventilation (Inolivent-8 prototype). CT images were taken at 1 and 2h30 of TLV, while subjects remained in supine position. Blood gas analyses were performed at the same times. The CT scan images, taken during expiratory pause, were segmented and analyzed with the 3D Slicer image computing open-source software to determine the pulmonary volume at each timepoint. Data is presented as median [Q1; Q3]. Friedman followed by Wilcoxon signed-rank tests were used.
Results:
At baseline, total lung volumes at end-expiration were measured at 44 [37; 49] mL/kg. Almost no air was present from 1h of TLV and thereafter. At 1 and 2h30 of TLV, the pulmonary volumes measured were higher, reaching 64 [57; 83] mL/kg (p=0.028) and 63 [55; 75] mL/kg (p=0.028), respectively. There was no difference in lung volume at these two timepoints (p=0.345). Qualitative analysis of the images reveals the distribution of perflubron during VLT favors the dependent lung regions. Blood gas at 2h30 of TLV were as follows: pH = 7.25 [7.21; 7.28], paO2 = 129 [99; 156] mmHg, paCO2 of 53 [48; 62] mmHg, and HCO3- = 21.4 [18.9; 24.6] mmol/L.
Conclusion(s):
Following the first hour of TLV, the total lung volume of perflubron can be maintained stable during at least 90 min. However, we believe the active process of fluid removal from the respiratory system during mechanical expiration needs to be refined to decrease total lung volumes during TLV. We also hypothesize that changing the position of subjects undergoing TLV could optimize this process.