Nephrology: Clinical
Nephrology 1: AKI
250 - Investigating the Use of Multi-agent Diuretic Regimens in Critically Ill Children with Suspected Fluid Overload
Publication Number: 250.25
Rosanna Fulchiero, DO
Pediatric Nephrology Fellow
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background:
Fluid overload (FO) is common in critically ill children and is associated with substantial morbidity and mortality, including: respiratory failure, longer intensive care unit (ICU) and hospital length of stay (LOS), and severe acute kidney injury (AKI) requiring continuous renal replacement therapy (CRRT). Diuretic medications are a cornerstone of therapy in FO, but the optimal approach remains unclear. Furthermore, at present, there is no literature evaluating the use of multi-diuretic regimens on important clinical outcomes (need for CRRT, LOS and mortality) in critically ill children with suspected FO.
Objective:
Explore the use of multi-agent diuretic regimens and associated clinical outcomes in critically ill pediatric patients with suspected FO.
Design/Methods:
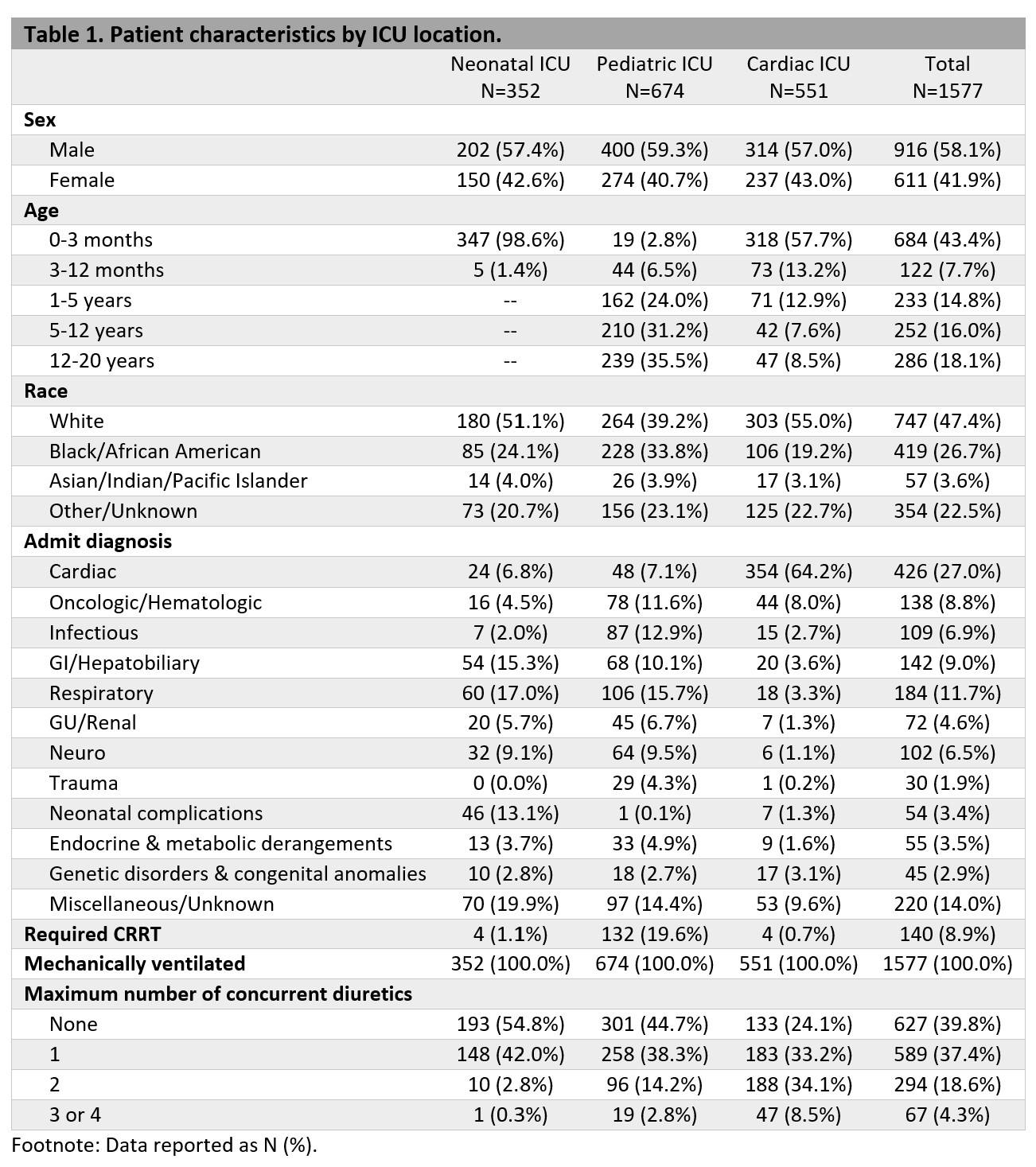
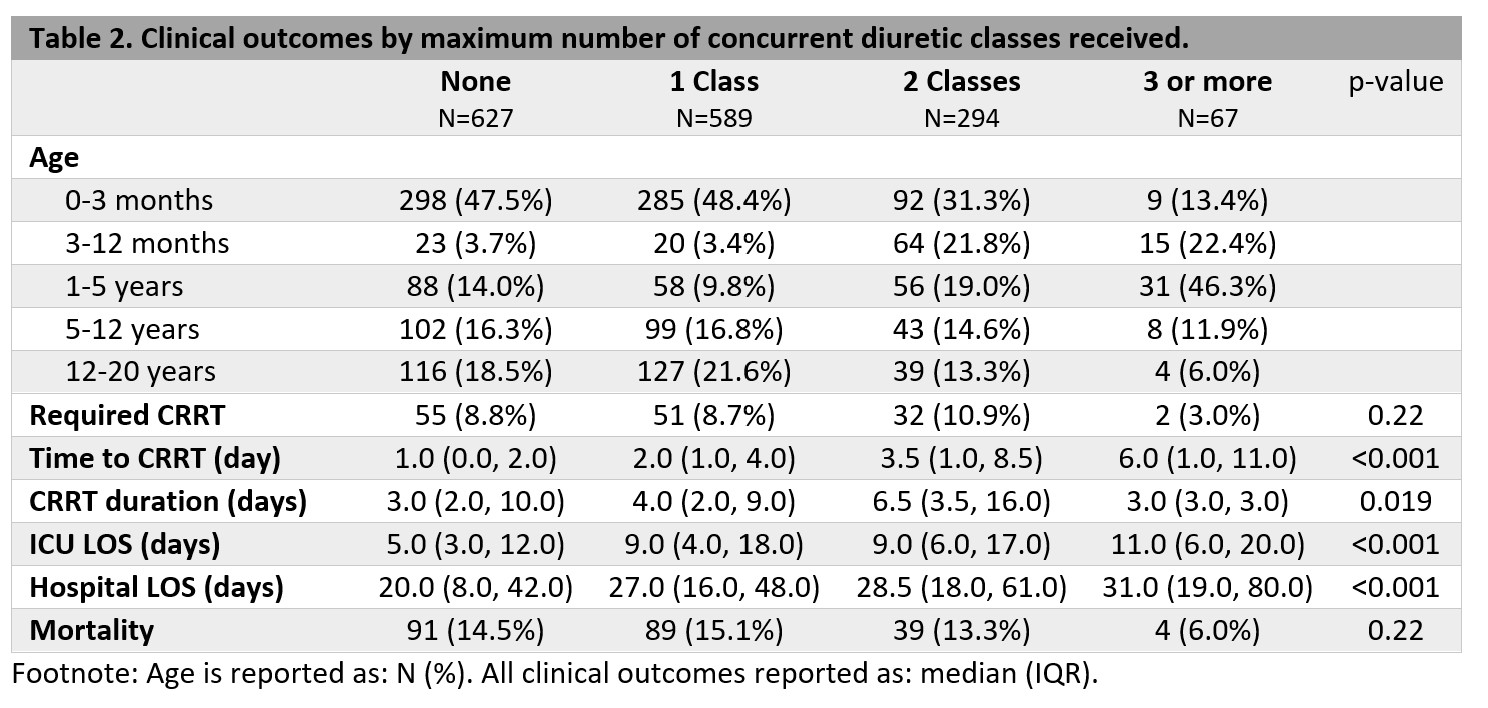
This is a retrospective cohort study of pediatric patients admitted to the ICU (pediatric, neonatal or cardiac) at a large academic children’s hospital from 2015 to 2022 with suspected FO based on a pre-existing algorithm within the electronic medical record. Patients were included if they experienced acute respiratory failure (need for invasive mechanical ventilation) with abnormal creatinine for age (combination validated in adult literature). Diuretic exposure was modeled as maximum number of concurrent diuretic classes administered during ICU stay. Classes included: loop diuretics, thiazide diuretics, spironolactone and metolazone. Clinical outcomes were compared between groups using Kruskal-Wallis or Pearson’s chi-squared tests as appropriate.
Results:
Of the 1,557 patients in the cohort, 60% received diuretics during ICU stay. Most received one class (62%), 31% received two and 7% received three or more concurrent diuretic classes. Sixty-eight percent of patients received loop diuretics, 23% thiazide diuretics, 7% spironolactone and 2% metolazone. Nearly half (47.5%) of patients that did not receive diuretics were age 0-3 months (Table 2), and patients hospitalized in the cardiac ICU were more likely to receive two or more concurrent diuretics than patients in the pediatric or neonatal ICU (Table 1). Median ICU LOS trended upwards with increase in concurrent diuretic use (5 vs 11 days, p< 0.001) as did median hospital LOS (20 vs 31 days, p< 0.001). There was no difference between groups in need for CRRT or mortality (Table 2).
Conclusion(s):
To our knowledge, this is the first study to explore the use of multi-agent diuretic regimens and associated clinical outcomes in critically ill children with suspected FO. Additional research is needed to inform optimal diuretic strategies to improve outcomes in this high-risk patient cohort.