Neonatal-Perinatal Health Care Delivery: Epidemiology/Health Services Research
Neonatal-Perinatal Health Care Delivery 3: Epi/HSR Antenatal Exposures and Neonatal Outcomes
751 - Maternal Pre-Pregnancy Obesity and Offspring Adolescent Blood Pressures After Extremely Low Gestational Age Birth
Publication Number: 751.246
- KS
Keia Sanderson, MD, MSc
Assistant Professor of Medicine and Pediatrics
University of North Carolina at Chapel Hill School of Medicine
Chapel Hill, North Carolina, United States
Presenting Author(s)
Background:
Maternal obesity is a risk factor for offspring obesity and adverse cardiovascular outcomes. Extremely premature (EP) infants are also at increased risk for adverse cardiovascular outcomes, including childhood hypertension. The extent of abnormal blood pressures (BP) in EP born children who are offspring of mothers with obesity is unclear.
Objective: To evaluate the association between maternal pre-pregnancy obesity on adolescent BPs among children born EP.
Design/Methods:
We were able to obtain 2 manual or oscillometric BPs in subsample of the Extremely Low Gestational Age Newborn (ELGAN) cohort (n=472; 39% of surviving participants), born 2002-2004. Study participants were 15-20 years old (mean age 17.8 years) at the time of BP measurements. Maternal pre-pregnancy weight and height were self-reported and other maternal factors were recorded from medical record. Seventeen ELGAN participants with BP measurements were excluded due to absence of maternal pre-pregnancy weight or height data.
Using linear regression modeling we evaluated the association between maternal pre-pregnancy obesity (Body Mass Index (BMI) ≥30) and offspring adolescent systolic BP(SBP). In secondary analyses we evaluated the relationship between maternal pre-pregnancy and offspring BMI, and offspring BMI and BP to evaluate if the relationship between maternal pre-pregnancy obesity BMI and offspring BP was associated with offspring BMI.
Results:
108 (24%) of the 455 adolescents were born to mothers with a history of pre-pregnancy obesity (BMI ≥30) (Table 1). Adolescents born to mothers with pre-pregnancy obesity had a greater median SBP of 120 mmHg (IQR 110,130) compared to adolescents born to mothers without obesity (SBP 115mmHg (IQR 107,1222)).
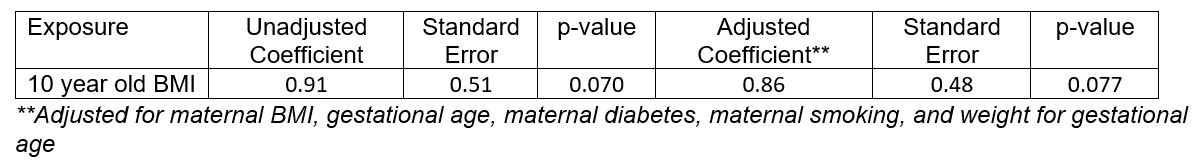
In the linear regression analysis, increasing maternal pre-pregnancy BMI was significantly associated with increasing offspring SBP (adjusted β coefficient 3.66, p=0.01) during adolescence. Increasing maternal pre-pregnancy BMI was also associated with offspring 10 year-old BMI (adjusted β coefficient 0.35, p=0.017). The association of offspring 10 year-old BMI and adolescent SBP was not statistically significant (adjusted β coefficient 0.86, p=0.077) (Tables 2-3).
Conclusion(s): For ELGANs, increasing maternal pre-pregnancy BMI was associated with increasing SBP and BMI in adolescence but pre-adolescent BMI was not associated with adolescent BP in this cohort. Future research directions include interventions to reduce maternal pre-pregnancy obesity with follow up of offspring BMI and BP as a way of reducing intergenerational cardiovascular risk.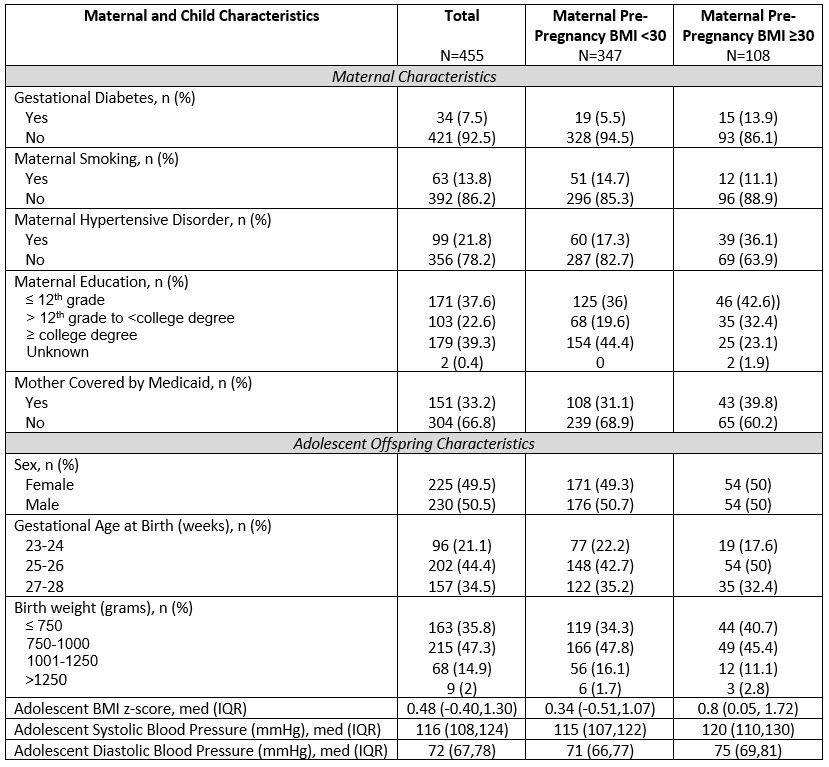
.jpg)