Back
Background: The decrease in oxygen to the tissues resulting from neonatal hypoxic-ischemic encephalopathy (HIE) leads to production of lactic acid. Potential therapies for metabolic acidosis include volume resuscitation such as boluses of normal saline (NS) or buffering agents such as bicarbonate or acetate. Both of these buffering medications are effective at improving pH, but they do not address the underlying cause of the acidosis and may cause paradoxical decrease in intracellular pH resulting in cell lysis in the already injured brain.
Objective: To evaluate the effect of bicarbonate or acetate compared to NS administration or no treatment (“control”) in normalizing pH, lactate, and base deficit (BD), and to assess the effect of administering buffering agents or NS on short-term outcomes.
Design/Methods: This retrospective cohort study included neonates born at ≥35 weeks of gestation, diagnosed with moderate or severe HIE, and admitted to the NICU at two centers 2012-2020. Neonates who did not receive hypothermia, who were placed on extracorporeal membrane oxygenation in the first 24 hours of life, or those with known central nervous system, cardiac, genetic, or chromosomal anomalies were excluded. Data collected included patient demographics and laboratory analyses obtained within the first 24 hours of life. Short-term outcomes collected included incidence of seizures, brain injury on MRI, or death prior to discharge.
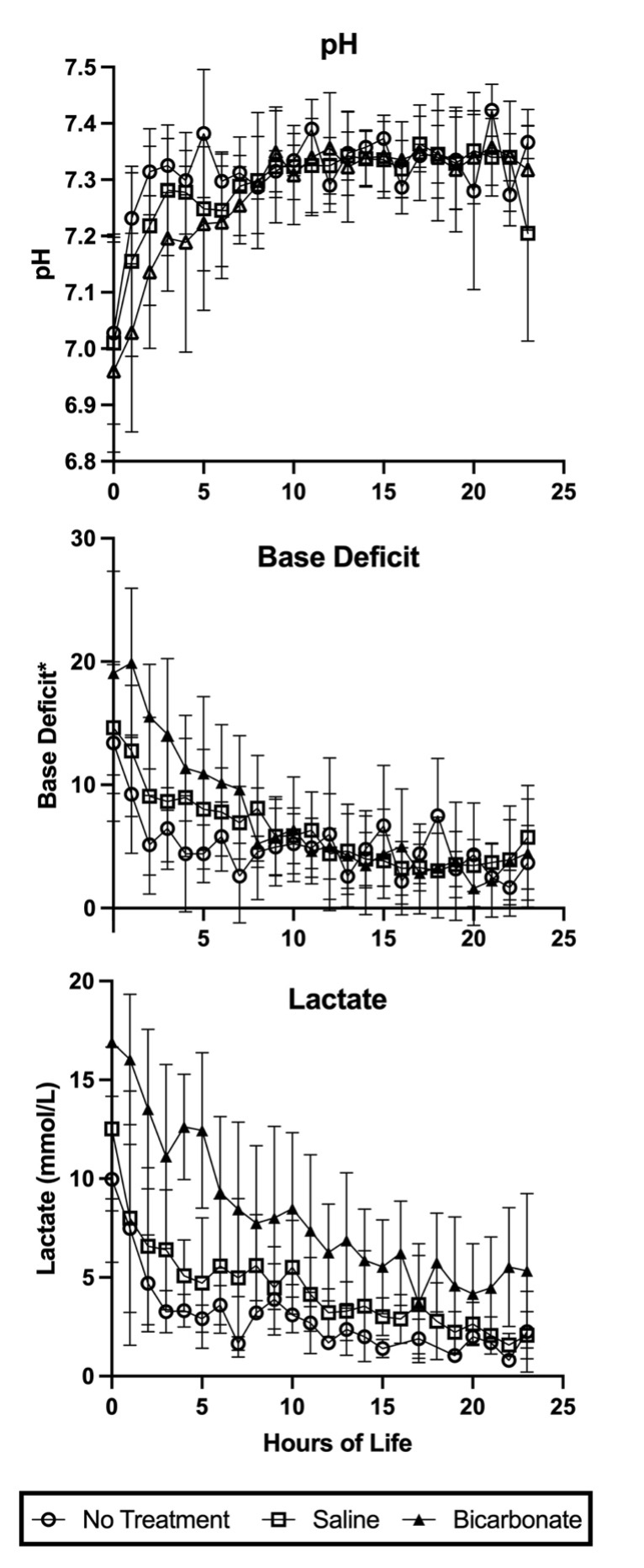
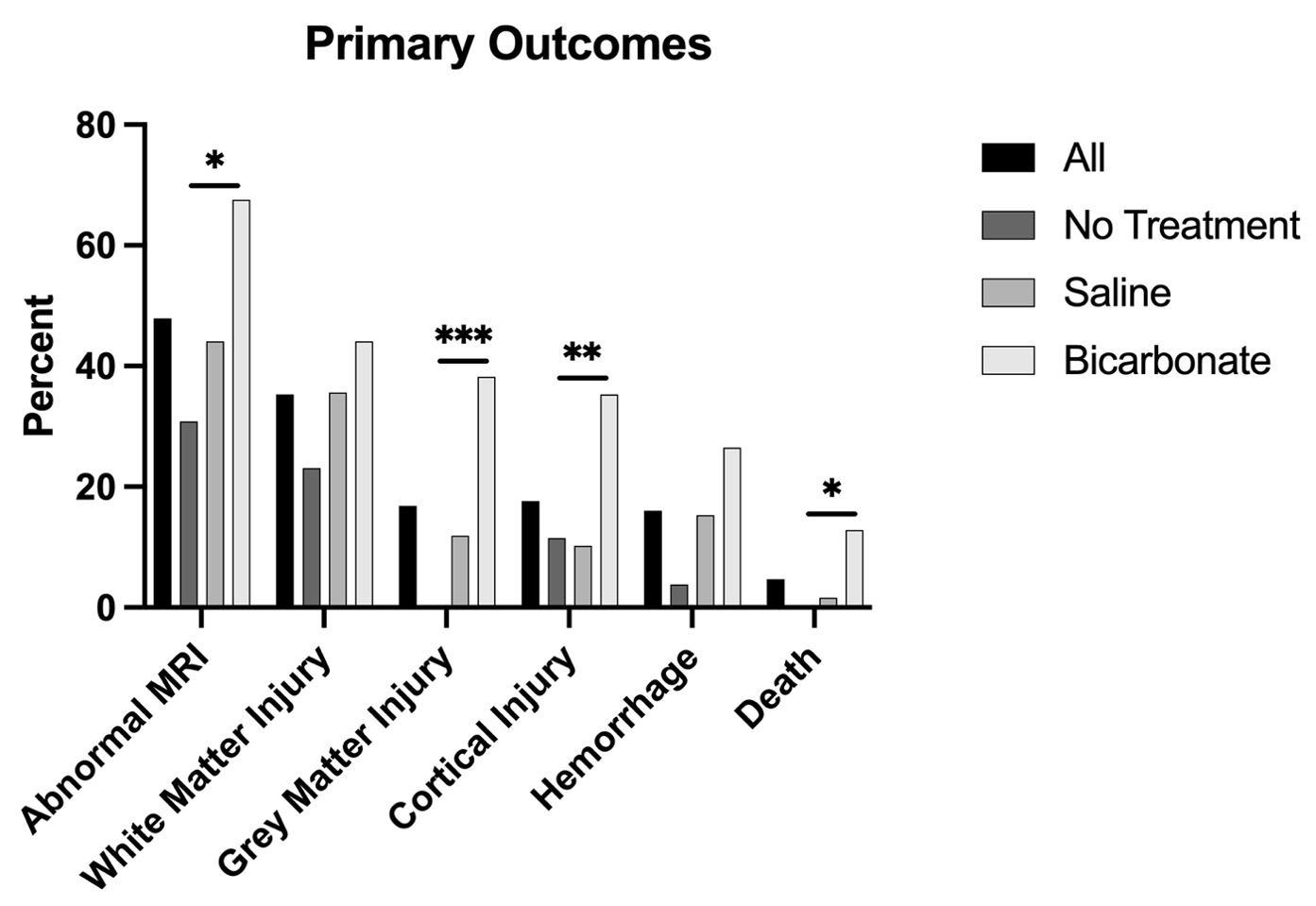
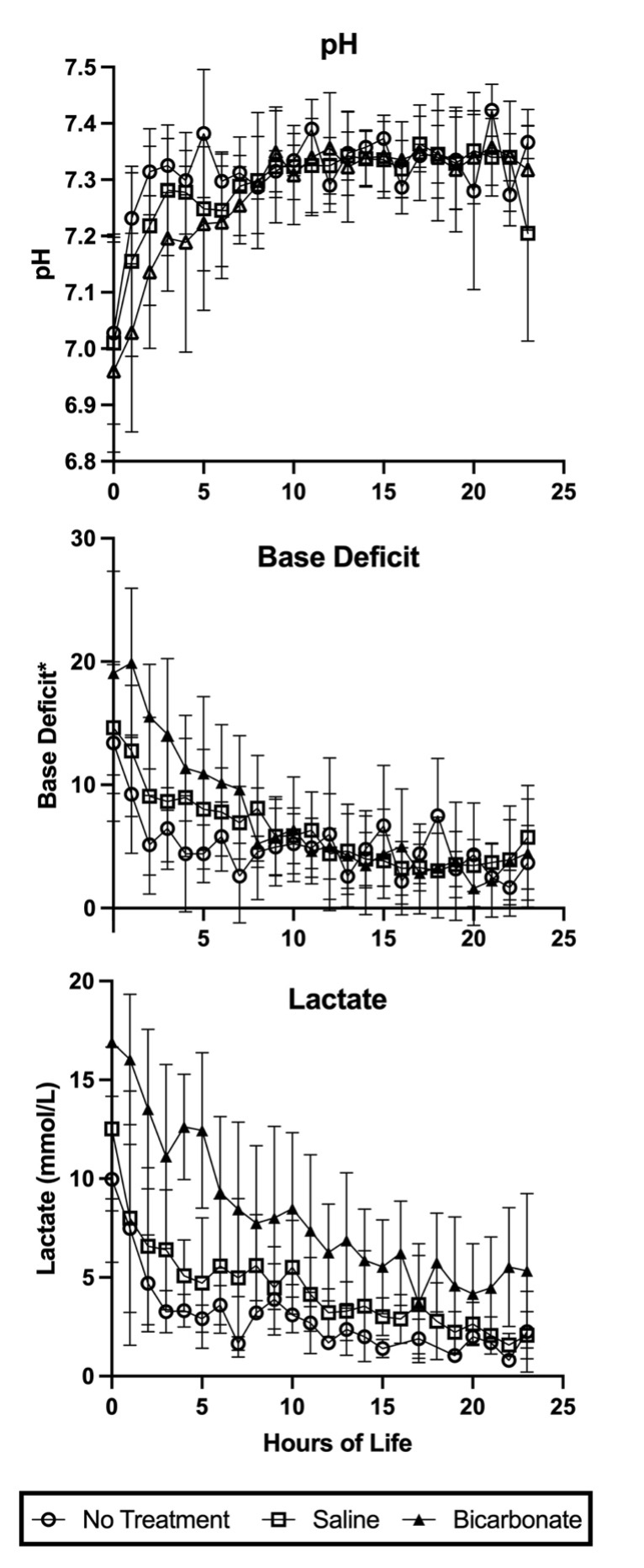
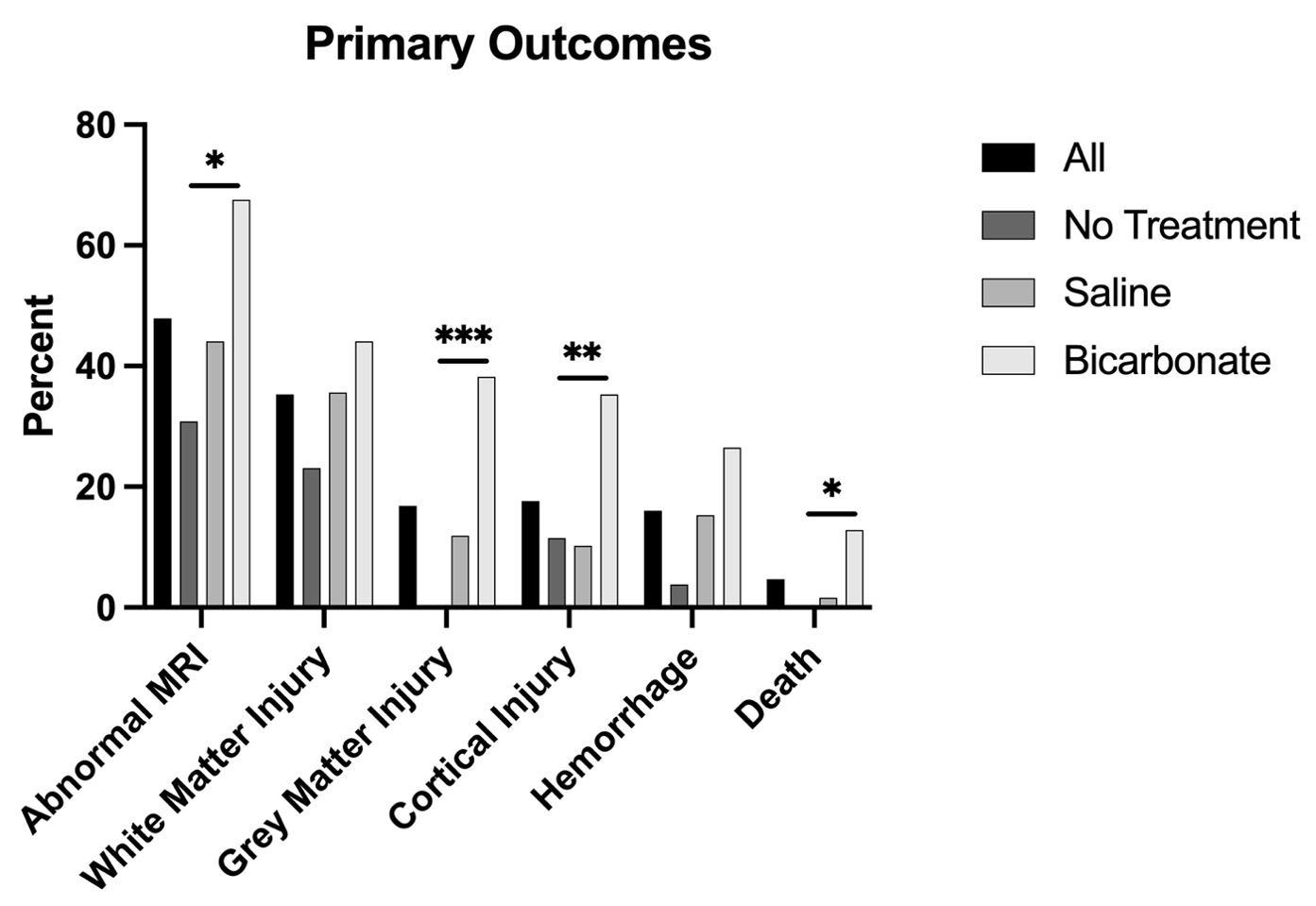
Results: Data were collected from 129 neonates: 39 in bicarbonate, 62 in NS, and 28 in control groups. Apgar scores at 5 (p=0.007) and 10 (p=0.002) minutes were the only demographics differing between the groups. There was no difference in baseline pH but higher baseline lactate and BD in the bicarbonate group compared to the control group (p=0.021 p=0.001, respectively, Fig.1). There was a longer time to normal pH within the bicarbonate group compared to the other two groups (p=0.001) but no difference in the time to normal lactate or BD. Death prior to discharge differed between all groups (p=0.025, Fig.2). On MRI, there was more injury on MRI (p=0.021) – primarily gray matter injury (p=0.001) and cortical injury (p=0.04) – in the bicarbonate compared to control group, though this was marginally significant when adjusting for 10 min Apgar scores (OR 3.03, p=0.085).
Conclusion(s): This study suggests bicarbonate use after HIE resulted in negative short-term effects as measured by death prior to discharge and brain injury on MRI compared to controls; however, bicarbonate treatment may have been used in more severe acidosis (i.e. initial lactate and BD derangements were more pronounced).
Neonatal Neurology: Clinical Research
Neonatal Neurology 2: Clinical 2
166 - Effect of Early Clinical Acidosis Management in Neonates with Hypoxic-Ischemic Encephalopathy
Friday, April 28, 2023
5:15 PM – 7:15 PM ET
Poster Number: 166
Publication Number: 166.136
Publication Number: 166.136
Erastus K. Thuo, Creighton University School of Medicine, Omaha, NE, United States; Elizabeth Lyden, University of Nebraska Medical Center, Omaha, NE, United States; Eric S. Peeples, University of Nebraska Medical Center, Omaha, NE, United States

Erastus K. Thuo, BA, MS
Medical Student
Creighton University School of Medicine
Omaha, Nebraska, United States
Presenting Author(s)
Background: The decrease in oxygen to the tissues resulting from neonatal hypoxic-ischemic encephalopathy (HIE) leads to production of lactic acid. Potential therapies for metabolic acidosis include volume resuscitation such as boluses of normal saline (NS) or buffering agents such as bicarbonate or acetate. Both of these buffering medications are effective at improving pH, but they do not address the underlying cause of the acidosis and may cause paradoxical decrease in intracellular pH resulting in cell lysis in the already injured brain.
Objective: To evaluate the effect of bicarbonate or acetate compared to NS administration or no treatment (“control”) in normalizing pH, lactate, and base deficit (BD), and to assess the effect of administering buffering agents or NS on short-term outcomes.
Design/Methods: This retrospective cohort study included neonates born at ≥35 weeks of gestation, diagnosed with moderate or severe HIE, and admitted to the NICU at two centers 2012-2020. Neonates who did not receive hypothermia, who were placed on extracorporeal membrane oxygenation in the first 24 hours of life, or those with known central nervous system, cardiac, genetic, or chromosomal anomalies were excluded. Data collected included patient demographics and laboratory analyses obtained within the first 24 hours of life. Short-term outcomes collected included incidence of seizures, brain injury on MRI, or death prior to discharge.
Results: Data were collected from 129 neonates: 39 in bicarbonate, 62 in NS, and 28 in control groups. Apgar scores at 5 (p=0.007) and 10 (p=0.002) minutes were the only demographics differing between the groups. There was no difference in baseline pH but higher baseline lactate and BD in the bicarbonate group compared to the control group (p=0.021 p=0.001, respectively, Fig.1). There was a longer time to normal pH within the bicarbonate group compared to the other two groups (p=0.001) but no difference in the time to normal lactate or BD. Death prior to discharge differed between all groups (p=0.025, Fig.2). On MRI, there was more injury on MRI (p=0.021) – primarily gray matter injury (p=0.001) and cortical injury (p=0.04) – in the bicarbonate compared to control group, though this was marginally significant when adjusting for 10 min Apgar scores (OR 3.03, p=0.085).
Conclusion(s): This study suggests bicarbonate use after HIE resulted in negative short-term effects as measured by death prior to discharge and brain injury on MRI compared to controls; however, bicarbonate treatment may have been used in more severe acidosis (i.e. initial lactate and BD derangements were more pronounced).