Quality Improvement/Patient Safety: Subspecialty-specific QI: see specialties above
QI 3: Subspecialty-specific QI & Patient Safety
701 - Reducing Safety Events During Transport of Critically Ill Pediatric Patients
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 701
Publication Number: 701.153
Publication Number: 701.153
Jillian Gregory, Maine Medical Center, Portland, ME, United States; Laura G. Amar-Dolan, Tufts University School of Medicine, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States; Kristine M. Pleacher, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States; Michael Zubrow, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States; Michael Ferguson, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States; Kirsten Orloff, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States; Jason Patregnani, The Barbara Bush Children's Hospital at Maine Medical Center, Cape Elizabeth, ME, United States; Asha S. Payne, Children's National Health System, Washington, DC, United States

Jillian Gregory, DO (she/her/hers)
Pediatric Intensivist
Maine Medical Center
Portland, Maine, United States
Presenting Author(s)
Background: Critically ill pediatric patients are transported from Maine hospitals to the pediatric intensive care unit (PICU) at the Barbara Bush Children’s Hospital (BBCH). BBCH is a tertiary care center serving Maine and Southern New Hampshire. As the frequency of safety events during transport was unknown prior to 2021, we implemented a transportation evaluation system to quantify and qualify safety events.
Objective:
We sought to improve the safety of PICU transport by reducing major and minor safety events through a quality improvement initiative.
Design/Methods:
After each patient transport, the PICU attending completed a survey tool to identify major and minor safety events. We defined major safety events as intubation, unintended extubation, or cardiac arrest. Minor safety events were defined as poor communication between facilities, equipment malfunction, initiation of vasoactives, hypotension, hypoxia, or increased sedation due to agitation. We developed process charts to track all safety events. Further, we analyzed the current system to identify high yield areas for interventions. During our 1st PDSA cycle, we instituted educational initiatives aimed at identifying and triaging critically ill children. During our 2nd, the existing transport checklist was reviewed and updated. Our 3rd PDSA cycle included changing the configuration of personnel on the PICU triage calls. During our last cycle, the EMR was updated for each patient to include triage call details. The main outcome measures were the types and number of safety events.
Results:
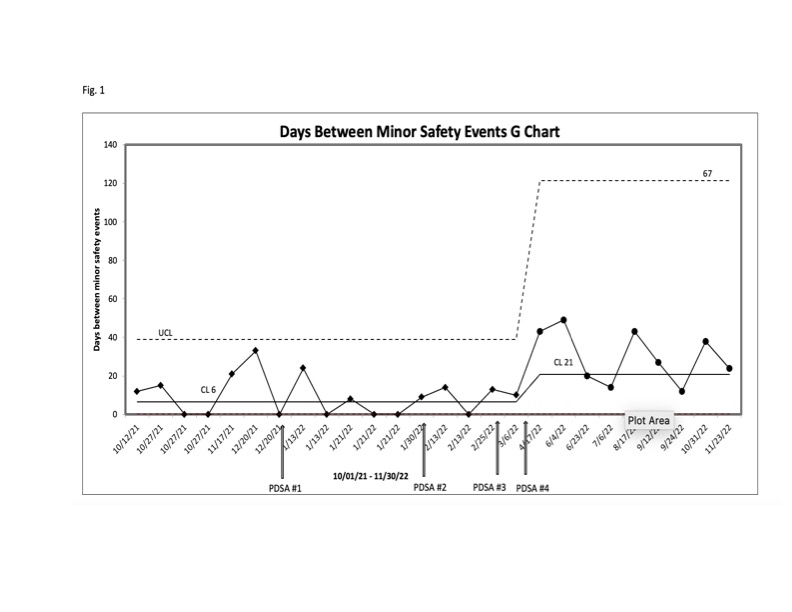
One hundred and forty-nine transports occurred over a 13-month period between October 1, 2021 and November 30, 2022. One major safety event and 26 minor safety events were recorded. Poor communication was the most common safety event (n=12, 46%). Given the low rate of minor safety events and a stable process identified during the first six months of data collection, a G Chart was utilized to track the number of days between minor safety events (Fig. 1). After our last PDSA cycle, we saw a sustained and significant increase in the number of days between safety events with a centerline shift from 6 to 21 days.
Conclusion(s):
Our quality improvement team successfully reduced the number of safety events at our institution over the project duration. Since communication issues resulted in the largest number of safety events, updating the EMR with diagnostic and therapeutic advice proved to be most impactful, as this information is available to access at most institutions. Further study into the benefits of shared EMR between referring and receiving facilities is warranted.