Neonatal Quality Improvement
Neonatal Quality Improvement 1
645 - Improving safety of non-emergent tracheal intubation in the neonatal intensive care unit: A quality improvement study
Publication Number: 645.138
.jpg)
Sara Neches, MD (she/her/hers)
Neonatology-Perinatology Fellow
University of Washington School of Medicine
University of Washington
Seattle, Washington, United States
Presenting Author(s)
Background:
Intubation premedication, including a paralytic, has been proposed to improve the success and safety of neonatal tracheal intubation (TI). As part of our participation in the National Emergency Airway Registry for Neonates (NEAR4NEOS), we track the occurrence of both severe and non-severe adverse TI associated events (TIAE). This quality improvement initiative has a global aim of optimizing provider use of full premedication (vagolytic+opiate analgesic+paralytic) for non-emergent TI at the Level IV neonatal intensive care unit at the University of Washington Medical Center.
Objective:
To increase provider use of full premedication for non-emergent neonatal TI by 20% by July 31, 2022.
Design/Methods:
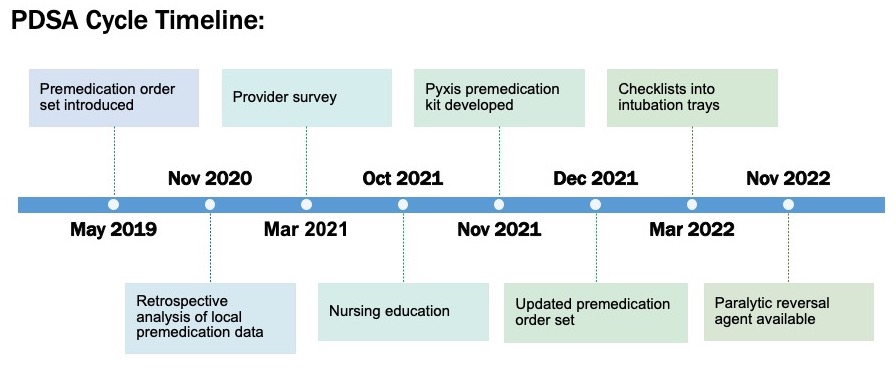
A review of baseline data, provider surveys, and discussions with key stakeholders revealed a lack of a timely medication administration process and concerns about medication dosage as significant barriers to using full premedication. A quality improvement team implemented process changes over multiple plan-do-study-act cycles, including electronic intubation order set, nursing education, development of a pyxis premedication kit, order set modification, and intubation checklist (Figure 1). The primary outcome was the quarterly usage of full premedication for eligible TI. Process measures included the quarterly rate of any TIAE. As balancing measures, we collected data on adverse medication events (e.g., rigid chest) and the need for medication re-dosing. We used statistical process control charts.
Results:
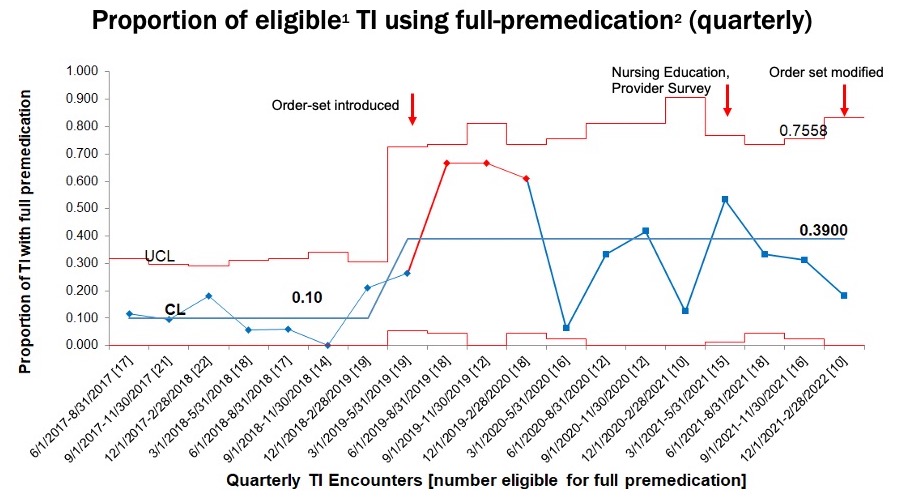
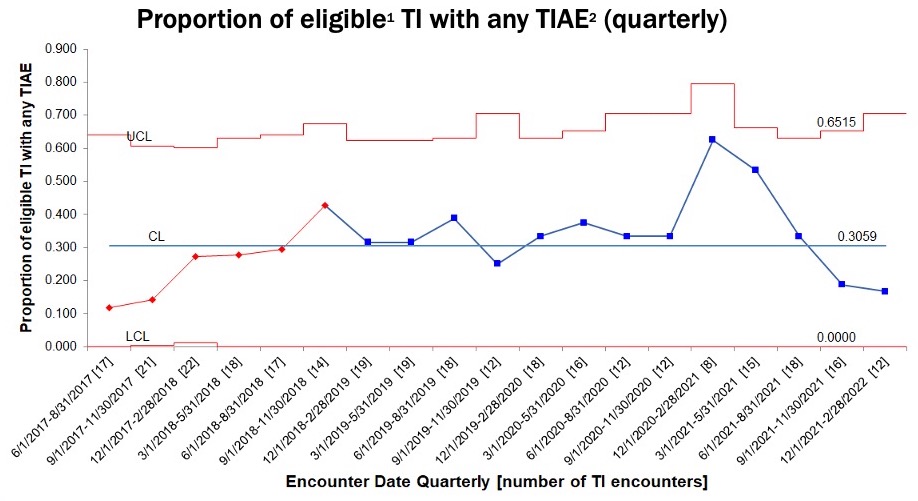
Data collection from June 2017-Feb 2022 included 362 first-course TI encounters in the NICU. We excluded TI occurring in the delivery room and in-unit TI in the setting of unstable hemodynamics such as ongoing cardiopulmonary resuscitation (CPR) or surfactant delivery via Intubate-Surfactant-and-Extubate (INSURE). Before interventions, an average of 0.10 (SD 0.07) eligible in-unit TI used full premedication. During the intervention phase, this increased to an average of 0.39 (SD 0.21) (Figure 2). The average quarterly rate of eligible TI with any adverse TIAE remained stable at 0.31 (SD 0.08) (Figure 3), and the quarterly rate of severe TIAEs remained stable at 0.06 (SD 0.05). There were no adverse medication events and no need for medication re-dose. Data collection is ongoing.
Conclusion(s):
Engaging an interdisciplinary QI team in an initiative focused on neonatal intubation safety has led to a 30% increase in the usage of full premedication for non-emergent TI without an increase in TIAEs. Future studies should explore provider hesitation and practice variation regarding use of full premedication.