Neonatal Neurology: Clinical Research
Neonatal Neurology 2: Clinical 2
173 - The impact of seizures in worsening brain injury after neonatal hypoxic ischemic encephalopathy: Interpretations from CNS-specific serum biomarkers
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 173
Publication Number: 173.136
Publication Number: 173.136
Raul Chavez-Valdez, Johns Hopkins University School of Medicine, CATONSVILLE, MD, United States; Jie Zhu, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Jordan R. Kuiper, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, United States; Khyzer B. Aziz, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Ernest M. Graham, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Christopher T. Campbell, Meso Scale Diagnostics, Gaithersburg, MD, United States; Carl E.. Stafstrom, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Frances J.. Northington, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Allen D. Everett, Johns Hopkins University School of Medic, Glenwood, MD, United States
Raul Chavez-Valdez, MD (he/him/his)
Associate Professor
Johns Hopkins University School of Medicine
Baltimore, Maryland, United States
Presenting Author(s)
Background: Despite therapeutic hypothermia (TH), a large proportion of neonatal hypoxic-ischemic encephalopathy (HIE) survivors suffer from long-term disabilities. In patients with HIE, seizures during the first 24 hours of life are evidence of moderate to severe encephalopathy. Though seizures are indicative of the degree of brain injury after HIE, it is unclear if seizure activity itself worsens brain injury.
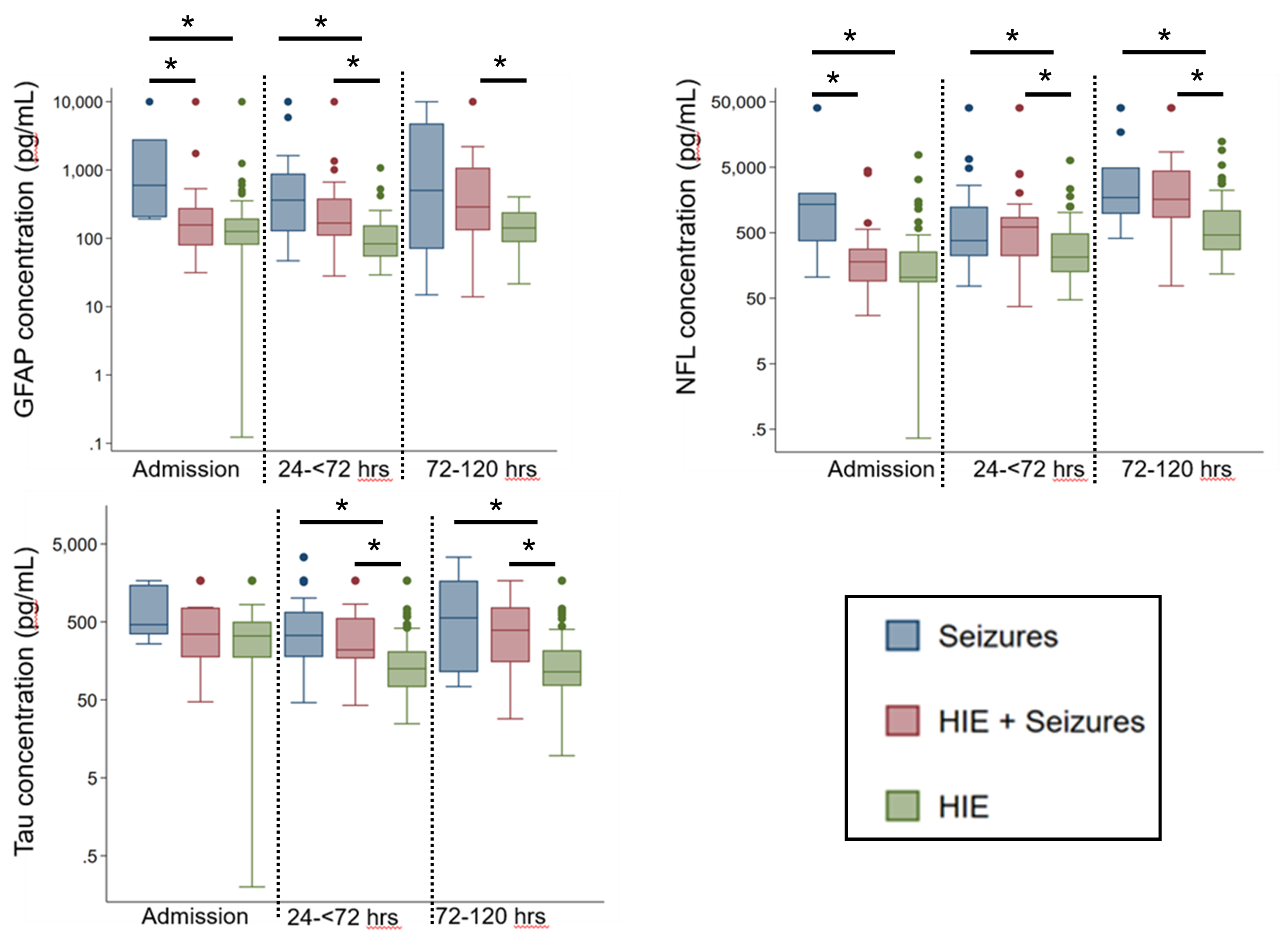
Objective: To test if CNS-specific serum biomarkers GFAP, NF-L and Tau would discriminate patients with and without seizures supporting that seizures may worsen brain injury.
Design/Methods: This was an IRB approved ancillary project from the prospective Biomarkers in Neonates (BIN) study, which collected remnant serum samples during the first 7 days since admission for neurological patients at the JHH NICU beginning in 2009. Here, we used a newly developed ultrasensitive Mesoscale Discovery platform to measure GFAP (astrocytic activation), NF-L (axonal degeneration) and Tau (neural cytoskeletal damage) in serum samples from 93 HIE/cooled patients: 68 without seizures (no Sz-HIE) and 25 who developed seizures (~90% within the first 24 hours; Sz-HIE), and compared them with 31 patients admitted during the first 72 hours of life for seizures but not HIE (Sz).
Results: Patients were on average 38.7 weeks gestation (SD± 1.8) , 3271 grams (SD ± 525 grams) and 57% were males, with no differences between the 3 subgroups. Strokes occurred in 39% of Sz patients and 3% of HIE patients. In Sz patients, GFAP at admission was 3.8 to 4.7-fold higher than levels in Sz-HIE (p=0.01) and no Sz-HIE (p=0.002) patients, while NF-L was 7.6 to 13-fold higher than levels in Sz-HIE (p=0.02) and no Sz-HIE (p=0.002) patients. During the next 72 hours (cooling period in HIE patients) concentrations of GFAP, NF-L and Tau did not differ between Sz and Sz-HIE patients. In contrast, higher levels of GFAP (4.3 and 2.1-fold), NF-L (1.8 and 2.9-fold) and Tau (2.7 and 1.8-fold) were detected in Sz and Sz-HIE patients than in no Sz-HIE patients respectively (p< 0.05 in all cases). Similarly, concentrations of all three biomarkers were greater among those with seizures compared to those without after 72 hours of life (Figure).
Conclusion(s): Relative to patients without seizures, concentrations of CNS-specific biomarkers linked to brain injury (GFAP, NF-L and Tau) were higher in those developing seizures. Concentrations were similar between patients in the Sz and Sz-HIE groups providing evidence to support the notion that seizures may worsen brain injury in patients with HIE.