Neonatal Neurology: Clinical Research
Neonatal Neurology 1: Clinical 1
157 - The Use of aEEG is Feasible for Enhanced Evaluation of Neonatal Encephalopathy in the Community Setting
Publication Number: 157.135
- SP
Silvia Patrizi, MD (she/her/hers)
Assistant Chief of Neonatology; Assistant Professor of Pediatrics
Harvard Medical School
Newton, Massachusetts, United States
Presenting Author(s)
Background:
Therapeutic hypothermia (TH) improves survival and neurodevelopmental outcome in infants with neonatal encephalopathy (NE). Rigorous and timely evaluation are needed for accurate selection of eligible patients. Several studies have reported worse outcome for outborn versus inborn infants. This difference could be attributed to variability in clinical practices, difficulties in monitoring markers of encephalopathy, and challenges in identifying eligible newborns within the first six hours of life. Although aEEG is a bedside neuromonitoring tool that improves early detection of NE as early as three hours of life, it is not routinely used in community hospitals.
Objective: The aim of this study was to assess the use of aEEG and the application of standardized guidelines to optimize the evaluation of neonates at risk of NE in a community hospital Special Care Nursery
Design/Methods:
Newton-Wellesley Hospital has 4000 deliveries/year, resulting in 600 admissions to the Special Care Nursery affiliated with Brigham and Women’s Hospital. Prior to the development of the Evaluation Guideline, most infants at risk for NE were transferred to the cooling center and in those evaluated and not transferred, there was large variation in care practices. A comprehensive evaluation process including the aEEG has been implemented since 2018. During that period, we revised guidelines, converted from using hydrogel electrodes to subdermal needles and conducted quarterly quality case reviews.
Results:
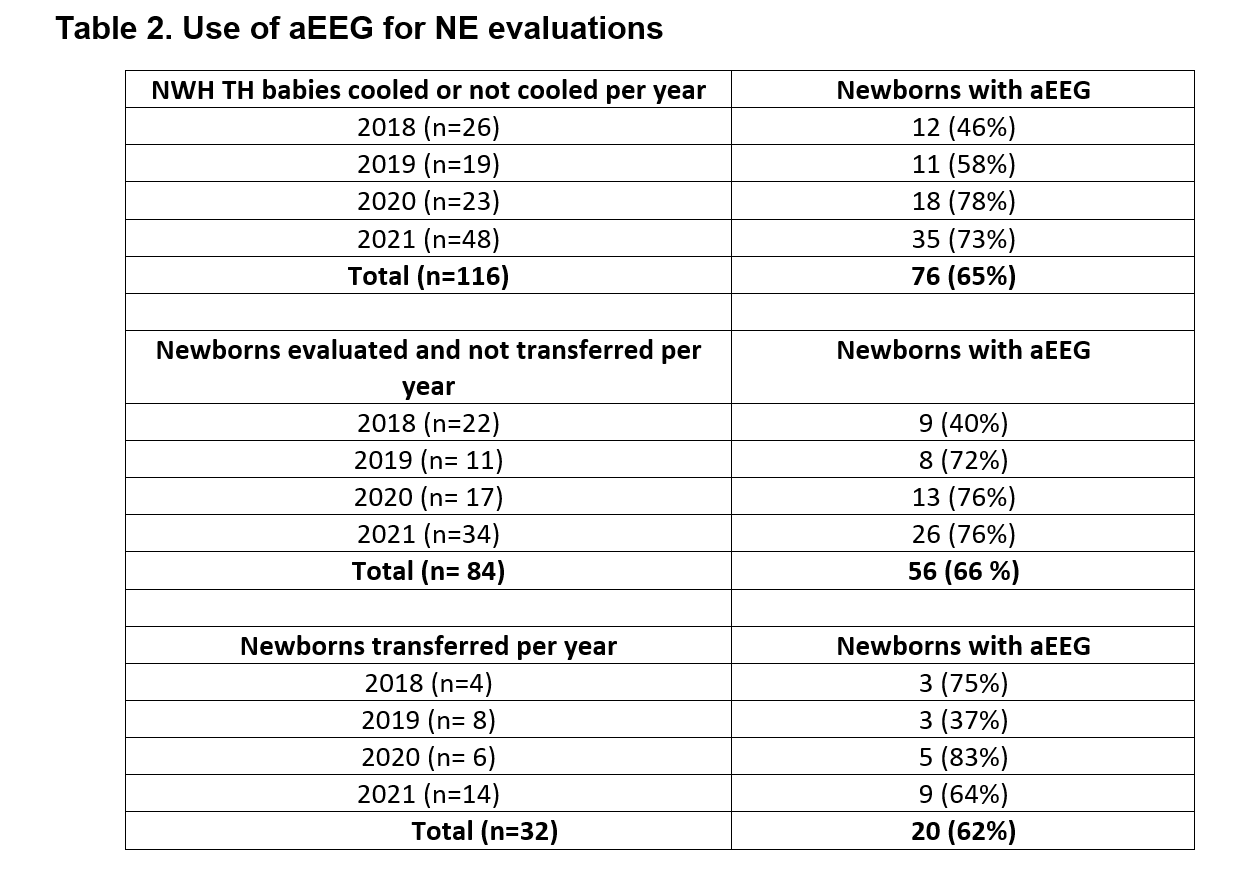
We evaluated 116 newborns at risk for NE from April 2018 to December 2021. Of the 116 newborns, 84 were evaluated and not transferred, and 32 were transferred to the cooling center. Standardized examination was used in 100% of infants. aEEG recording occurred in 65% of newborns (66% of those not transferred and 62% of those transferred). Placenta pathology was obtained in 97% of transferred patients. Transfers occurred at 3.5 h of life. Active cooling started at 5.1 h, with target temperature achieved at 5.4 h of life. 75% of transferred newborns were eligible for TH and received 72 h cooling.
Conclusion(s):
The use of clinical guidelines and aEEG can support clinicians in SCN to conduct accurate evaluation and selection of patients at risk of NE without delaying the start of TH. The potential benefits are early identification and transfer of patients eligible for TH to cooling centers within the therapeutic window; minimize mother-newborn separation and unnecessary procedures. The use of aEEG in the community setting is feasible and offers important information with the clinical decision process in a community hospital.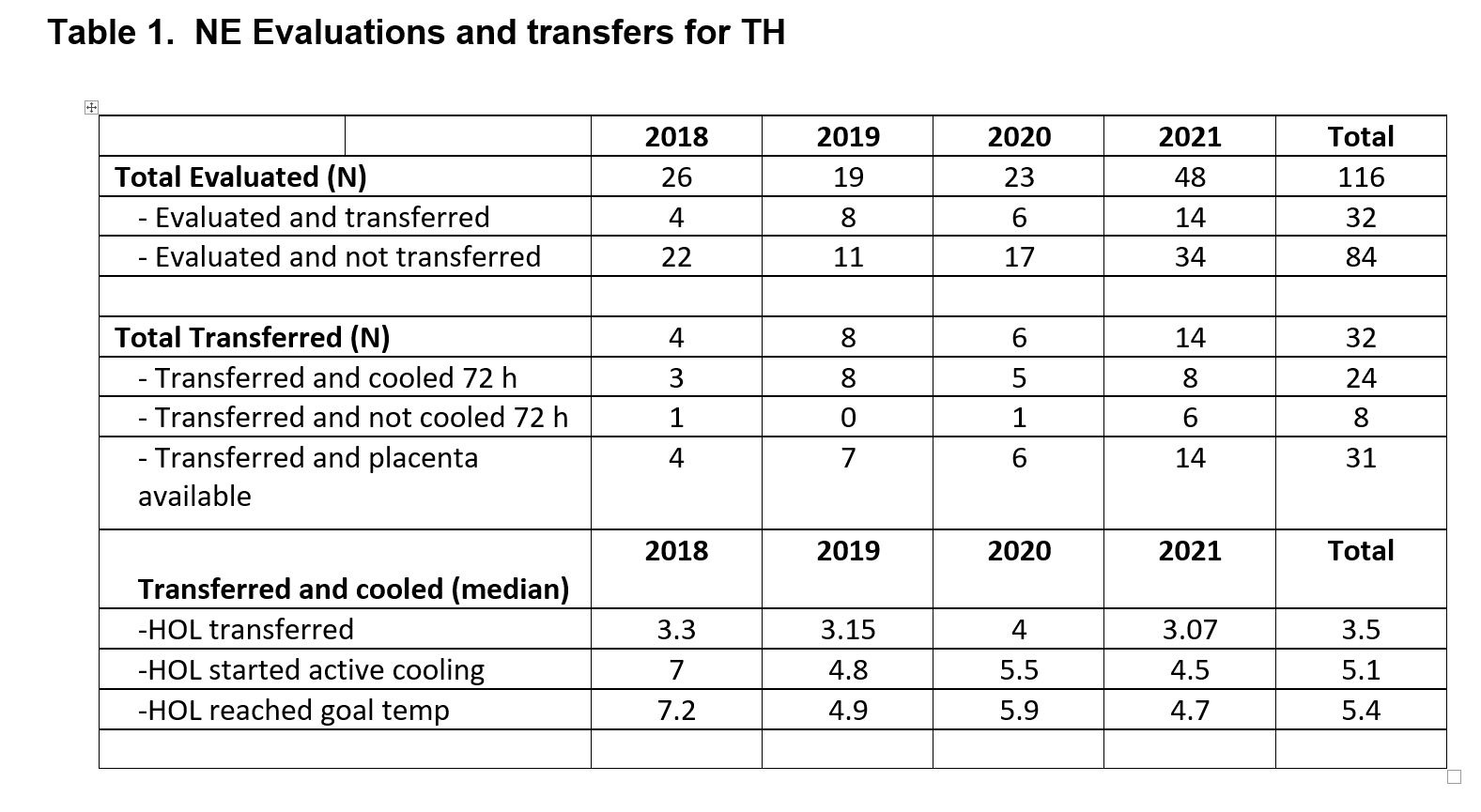
.png)
