Palliative Care
Palliative Care
431 - Design and Evaluation of a Pediatric Hospice/Palliative Medicine Curriculum
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 431
Publication Number: 431.147
Publication Number: 431.147
Ingrid Frydson, Baylor College of Medicine, San Antonio, TX, United States; Hollie Statzer, Baylor College of Medicine, San Antonio, TX, United States; Ruchi Kaushik, The University of Texas Health Science Center at San Antonio Joe R. and Teresa Lozano Long School of Medicine, San Antonio, TX, United States
.jpg)
Ingrid Frydson, MD
Pediatric Resident
Baylor College of Medicine
San Antonio, Texas, United States
Presenting Author(s)
Background: Gaps remain in resident hospice/palliative medicine (HPM) education. We conducted a targeted, local needs assessment to better understand pediatric resident HPM curricular priorities that informed our design of a pediatric HPM curriculum.
Objective:
- To design and evaluate a pediatric resident HPM curriculum using our local needs assessment results.
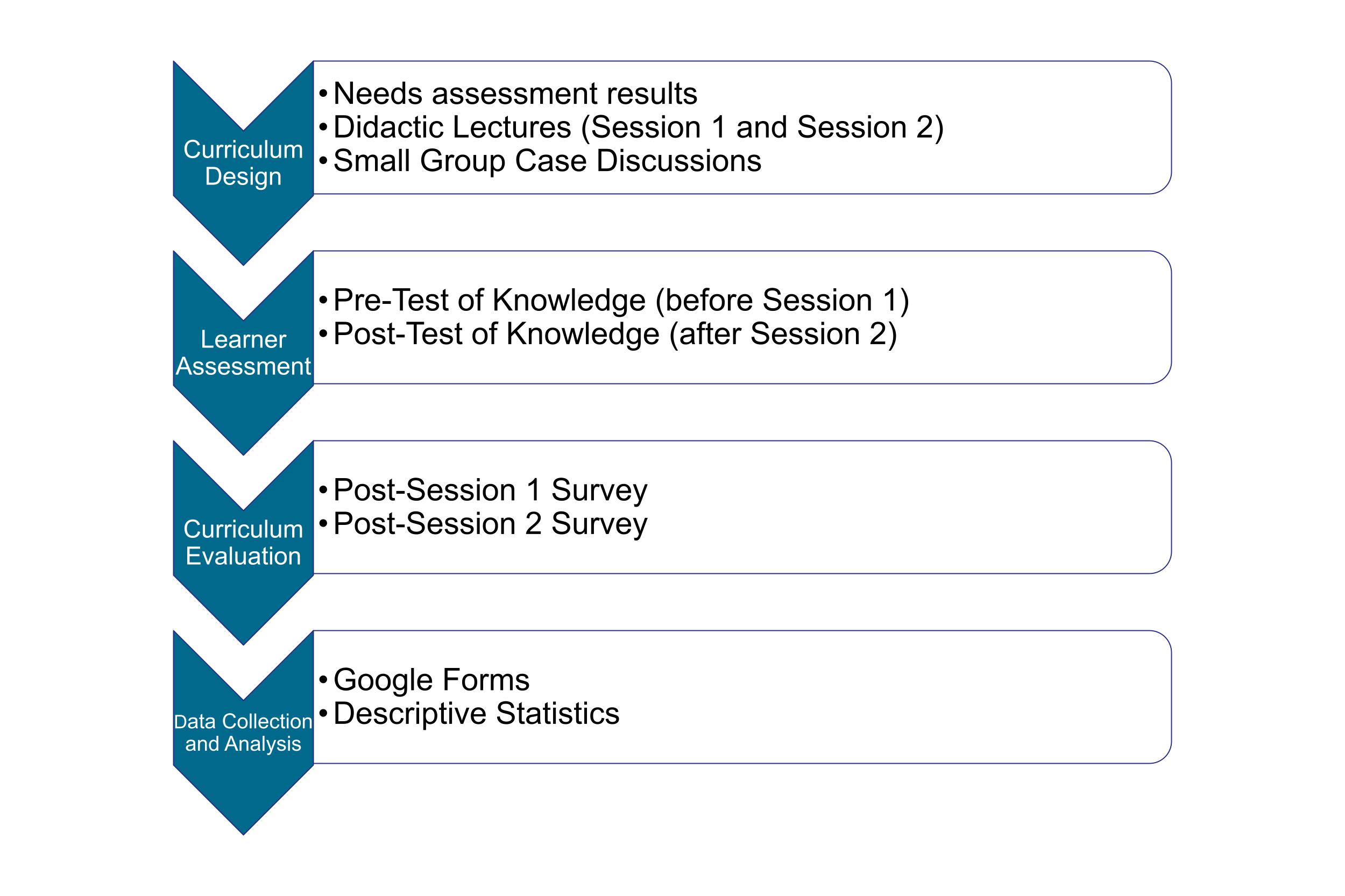
Design/Methods: We formulated educational objectives, assembled didactic lectures to deliver evidence-based palliative care communication skills (session 1) and pediatric pain evaluation and management practices (session 2), and developed relevant cases to allow pediatric residents to practice newly-learned skills. Residents completed a pre-test prior to session 1, a post-session 1 survey, a post-test following session 2, and a post-session 2 survey.
Results: We delivered sessions 1 and 2 to 34 and 30 residents, respectively. Residents demonstrated a statistically significant difference in pre- (n=34/34, 100%) and post-test (n=12/30, 40%) scores (54.4%, SD 0.15 vs 75%, SD 0.12, p=0.0001). Among 34 session 1 participants, 19 (55.9%) completed the post-session 1 survey. On average, 98.7%of residents reported the session met the four educational objectives “a lot,” “quite a bit,” or “a moderate amount.” Additionally, 73.7% reported feeling “extremely,” “quite,” or “moderately comfortable engaging in end-of-life and palliative care discussions.” Among 30 session 2 participants, 16 (53.3%) completed the post-session 2 survey. For all three educational objectives, 100% of residents reported the session met the objective “a lot” or “quite a bit.” Additionally, 93.8% and 100% reported feeling “extremely,” “quite,” or “moderately comfortable” in assessing pain in children with severe neurologic impairment (SNI) and formulating an initial pain management plan for children with SNI, respectively. For sessions 1 and 2, 94.4% and 100% found the session to be “extremely,” “quite,” or “moderately relevant” and 84.2% and 93.3% believed the session to be “extremely,” “quite,” or “moderately engaging”. Residents shared several curriculum strengths and opportunities.
Conclusion(s): A pediatric resident palliative care curriculum designed to address targeted needs assessment-identified curricular priorities met session objectives well. Delivery of the curriculum resulted in comfort in engaging in end-of-life and palliative care discussions, assessing pain in children with SNI, and formulating an initial pain management plan for children with SNI. Sessions were found to be relevant and engaging. Residents offered several qualitative comments to aid in curricular enhancement.
.jpg)
.jpg)
