Child Abuse & Neglect
Child Abuse & Neglect 2
604 - A Potential Situation for Optimism: Outcomes in Children Over Age 2 After Abusive Head Trauma
Publication Number: 604.104

Marcella M. Donaruma, MD (she/her/hers)
Associate Professor of Pediatrics
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background:
Morbidity and care expectations after hospitalization for abusive head trauma (AHT) can be significant for both abuse survivors and their caregivers.
Objective: This study describes the short- and long-term clinical outcomes for children who suffered abusive head trauma after infancy. We also identify clinical and psychosocial characteristics associated with those outcomes.
Design/Methods:
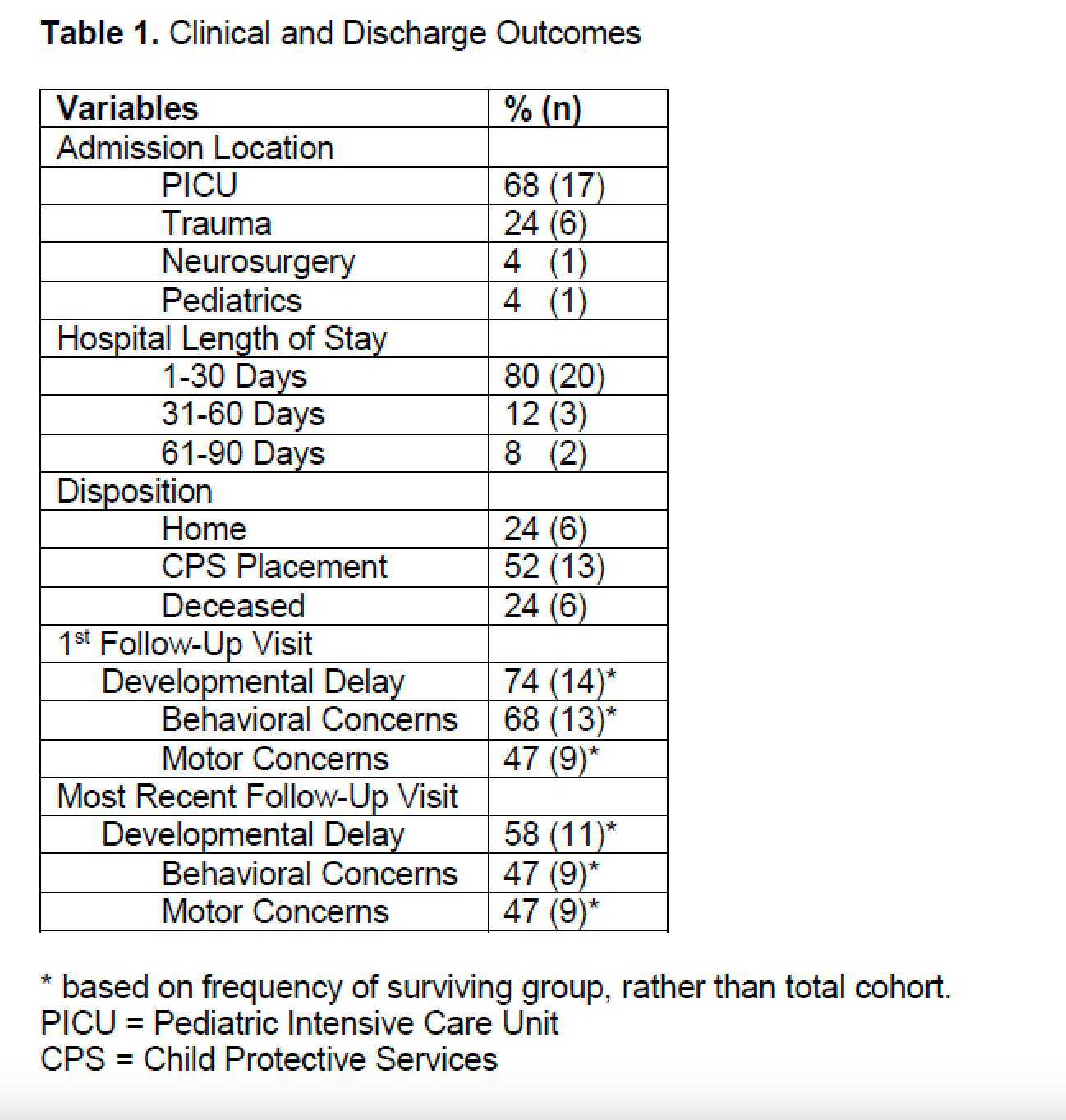
Retrospective case series of 25 children > 24 months old at the time of AHT diagnosis seen at a tertiary academic pediatric center from 2013 to 2021. Diagnosis confirmed by experts in Child Abuse Pediatrics. Follow-up in multidisciplinary clinics included Physical Medicine & Rehabilitation, Neurology & Development, Child Abuse Pediatrics and Social Work. Clinical and Social Vulnerability Index measures were also extracted. Exclusion criteria were age < 24 months and/or a plausible injury mechanism Developmental deficits were assessed from clinical documentation of standardized developmental testing of cognitive, language, and motor skills (the Capute Scales, including the Cognitive Adaptive Test (CAT) and the Clinical Linguistic and Auditory Milestone Scale (CLAMS), and the Bayley IV gross and fine motor screening). When developmental testing was not available, developmental outcomes were based on documentation of specific and standardized milestones.
Results:
Mean age at presentation was 45 months, 72% male. Six children (24%) died from their injuries. Surviving children went to relative or foster caregivers at discharge in 68% of cases, with 4 (21%) ultimately adopted. The remaining 32% survivors returned to their original homes. Three (16%) male AHT survivors re-experienced physical abuse after care by a biological parent resumed. At initial post-discharge evaluation, 74% of survivors showed cognitive and language deficits. Caregivers described aggression, tantrums, and regressive behaviors for 68% of children. Gross and fine motor delays were observed in 47%. At the most recent visit (mean 741.53 days post discharge), 58% of children had ongoing deficits. However, lower functional outcomes occurred for children with the greatest number of social stressors (n=5).
Conclusion(s):
Older AHT survivors gained improvements in early developmental delays and behavioral concerns over time, with the exception of motor skill acquisition. Factors indicating increased social vulnerability were associated with diminished gains post discharge, identifying a potential opportunity for intervention to maximize potential.