Children with Chronic Conditions
Children with Chronic Conditions 1
715 - Effects of an Individualized Home Assessment on Emergency Preparedness of Families of Children and Youth with Special Health Care Needs
Publication Number: 715.105

Renee Turchi, MD, MPH, FAAP (she/her/hers)
Chair of Pediatrics and Pediatrician in Chief
St. Christopher's Hospital for Children
Drexel University College of Medicine and School of Public Health
Abington, Pennsylvania, United States
Presenting Author(s)
Background:
Children and youth with special health care needs (CYSHCN) are a diverse and growing population with conditions that require specific planning and accommodations to minimize harm in an emergency or disaster.
Objective: Assess the effects of an interdisciplinary home assessment on the preparedness of families with CYSHCN.
Design/Methods:
A team of clinical providers, preparedness experts, social workers, community health workers, and durable medical equipment providers developed a comprehensive, 2-stage survey instrument addressing indicators of preparedness across fire safety, readiness for evacuation and sheltering in place (SIP), and access of emergency care providers to the CYSHCN’s medical information. Eligible participants resided in Pennsylvania and cared for CYSHCN with technology reliance, impaired physical mobility, communication or intellectual challenges, vision/hearing loss, or a combination of these. Families received emergency planning templates tailored to the CYSHCN’s medical condition(s) and information on local resources. Additional needs were addressed directly or through referrals to community supports. The survey instrument was re-administered at 3 to 6 months to evaluate whether preparedness metrics had changed.
Results:
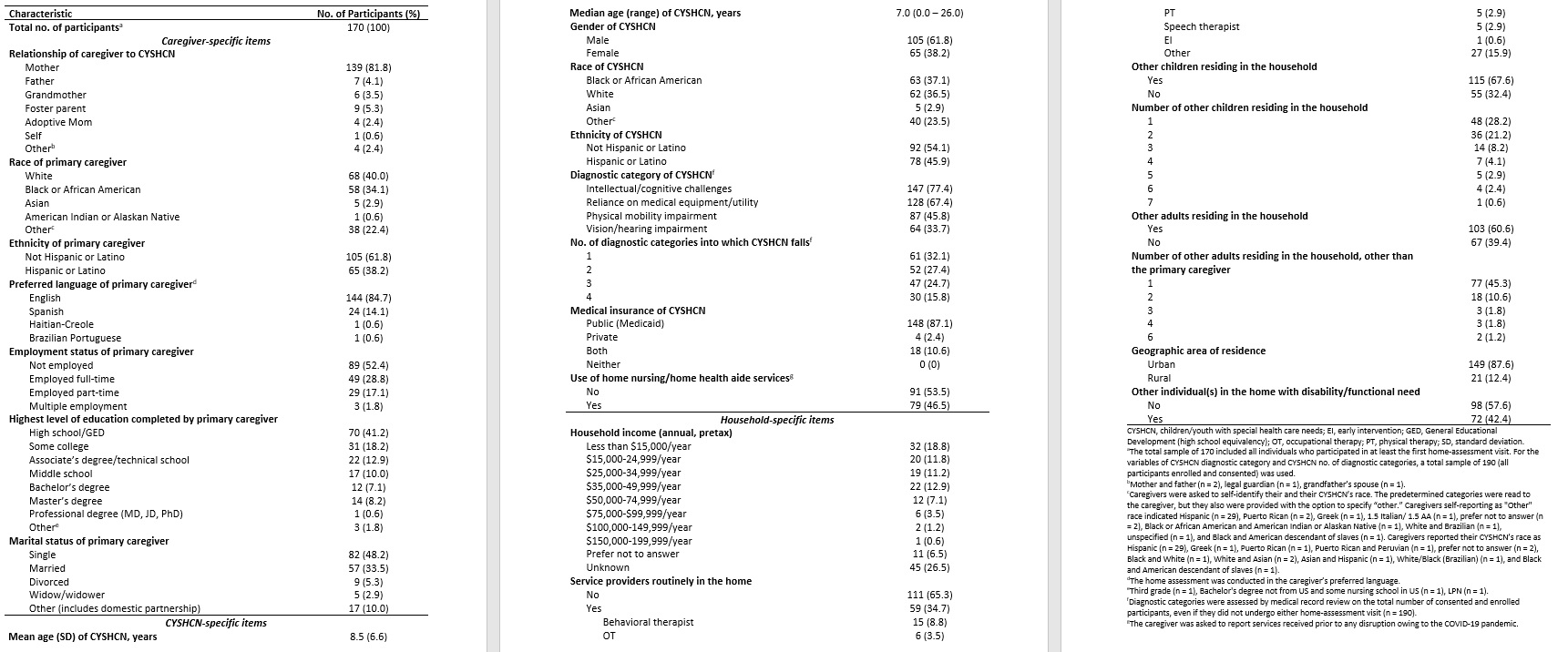
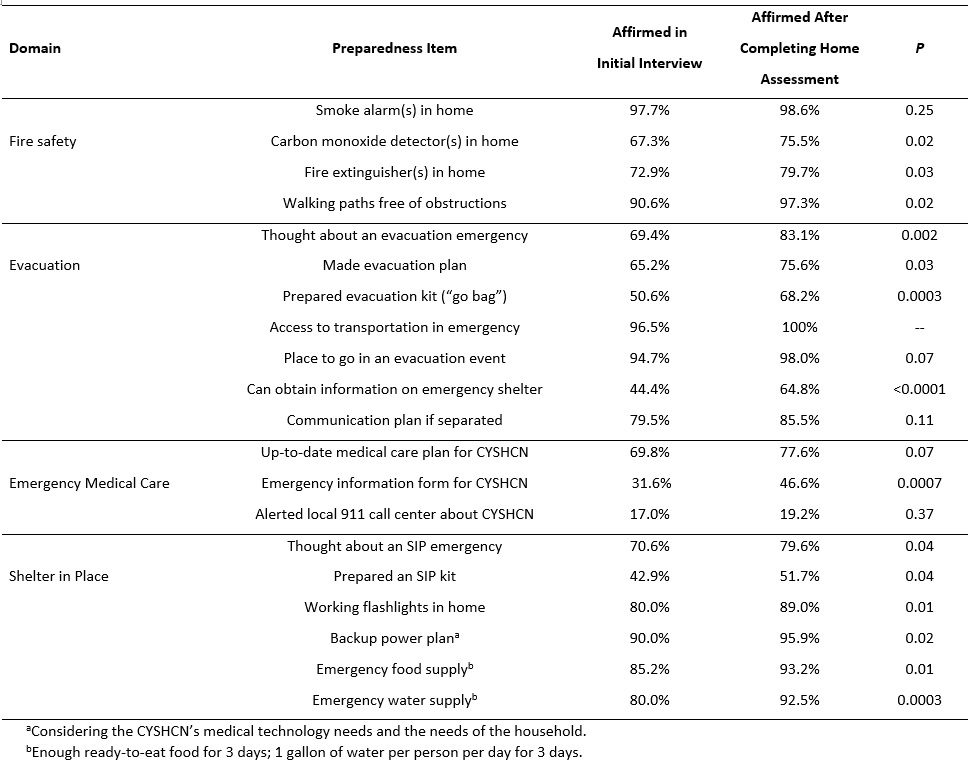
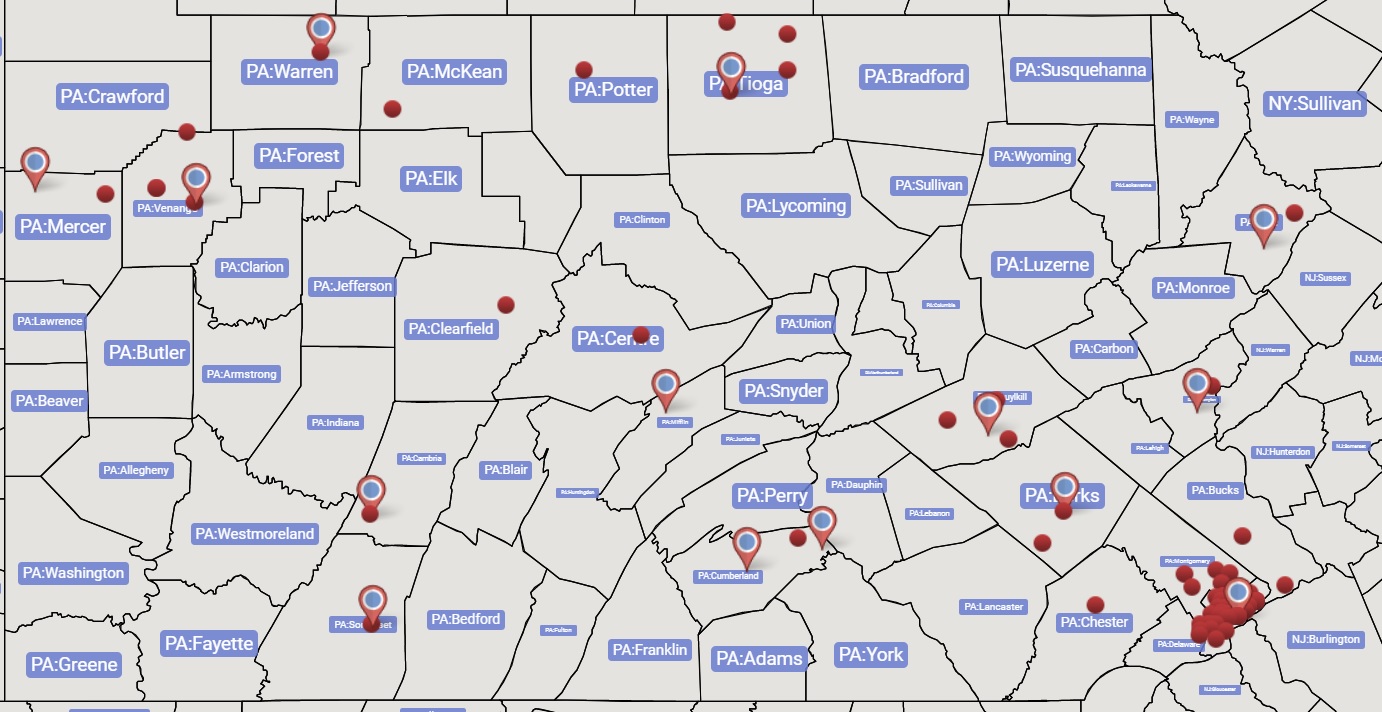
Caregivers (n = 190) were enrolled from April 2020 to January 2022; 68% of the CYSHCN had ≥2 of the 4 diagnostic categories (Table 1). Of the 170 who completed the initial home assessment (Figure 1), 82% were mothers, 40% identified as White (34% as Black), and 85% spoke English. Mean age of the CYSHCN was 8.5 years, 62% were male, 37% were Black (36% White), and 87% had public medical insurance. Among the 148 caregivers who completed the follow-up assessment, significant improvement was found in 15 indicators of basic preparedness, including having fire extinguishers, carbon monoxide detectors, and flashlights in the home; preparing an evacuation bag and an SIP kit; keeping emergency food and water supplies; creating a backup power plan; and having an up-to-date emergency information form and medical care plan (all p < 0.05; Table 2).
Conclusion(s):
An individualized home assessment with linkage to resources was associated with improved preparedness in families of CYSHCN. Future studies are needed to assess the impact of this intervention in a larger sample of families with CYSHCN. Partnerships are ongoing to assess replicability and scalability across PA and beyond.